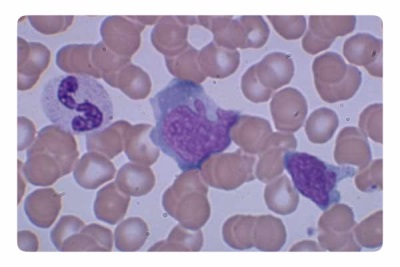
Atypical mononuclear cells in the blood of a child
All parents know that cells such as red blood cells and white blood cells and platelets are present in the child’s blood. Many mothers also know that leukocytes are represented by different species, and determining their level as a percentage is leukocyte formula.
What is it
Atypical mononuclear cells (their other name is “virocytes”) are modified mononuclear blood cells. In terms of their structure and function, virocytes can be attributed to white blood cells. Such cells have similarity with normal mononuclear cells - monocytes and lymphocytes.
In atypical mononuclear cells there is one core, which is distinguished by polymorphism and spongy structure. The shape of such cells is round or oval. Depending on the composition of the cytoplasm and the size of these cells are divided into monocyto- and lymphocyte-like.
According to many scientists, atypical mononuclear cells are derived from T-lymphocytes. They are produced in response to the penetration of viruses into the children's body or under the influence of other factors.
How to determine children
Detection of atypical mononuclear cells in children occurs during a clinical analysis of blood, including leukogram. Such cells are counted in the analyzed blood volume, compared with the number of all leukocytes and expressed as a percentage. The child is sent for this analysis:
- Planto make sure there are no hidden diseases.
- If there are complaints and if the doctor suspected an infection on the basis of an examination.
- In preparation for the operationand in some cases before vaccination.
- During exacerbation chronic pathologies.
- In the process of treatment to verify its effectiveness or inefficiency.
Norm
The reasons for the increased level
Most often, the level of atypical mononuclears increases with viral diseases, for example, with chickenpox. An increased percentage of virocytes is also detected when:
- Tumor processes.
- Autoimmune diseases.
- Pathologies of blood.
- Poisoning.
- Long-term use of certain drugs.
It should be noted that in most cases such cells do not exceed 10% of all leukocytes. If atypical mononuclear cells in the leukocyte formula of the blood test of children reveal more than ten percent, it is a reason to diagnose a disease in a child called "Infectious mononucleosis". Since its cause is Epstein-Barr virus, this disease is also called VEB infection.
With such an infection, atypical mononuclear cells are always detected in the child’s blood. The disease is more often diagnosed in children older than a year, and its incubation period can be up to two months, and you can become infected both through direct contact with a sick child and by airborne droplets. With this pathology, the level of atypical mononuclear cells can reach 50% of all leukocytes, and in some cases it is even higher.

The disease affects the lymphoid tissue, so children with infectious mononucleosis are diagnosed with inflammation of the tonsils, lymph nodes, spleen, and liver. The first symptoms of pathology are high body temperature, swollen lymph nodes, severe sore throat, nasal congestion. Virocytes appear in the blood of a sick child not immediately, but only after two or three weeks. In addition, they remain in the bloodstream of children for five to six weeks after recovery.
What to do with a high level in the blood
If a child’s blood test showed a high content of atypical mononuclear cells, this is a reason for going to a doctor. The pediatrician will evaluate the general condition of the baby, as well as the illness, since after a recent viral infection, the level of virocytes in the blood is elevated for several more weeks.
Having confirmed the presence of VEB infection in the child, he will be prescribed symptomatic therapy, including febrifugal, general strengthening, antiseptic and other drugs. There is no specific treatment for the Epstein-Barr virus.
In most cases, the prognosis of EBV infection is favorable and many children tolerate it in a mild form. Only some children have such serious complications as hepatitis, spleen rupture or laryngeal edema.
If the liver is damaged, the child is transferred to a special, sparing diet, supplementing it with drugs with hepatoprotective and choleretic action. If a bacterial infection has joined, the use of antibiotics and probiotics is indicated. In case of severe course or complications, the child may be prescribed hormonal agents, spleen removal, tracheostomy or artificial lung ventilation.