5 week of pregnancy: what happens to the fetus and the expectant mother?
The fifth obstetric week of pregnancy is special. It is during this period that most women learn that they will soon become mothers. That is why this week is remembered for many years. About what is happening with the baby and the future mother, we will tell in this material.
How many months is it
5 obstetric week of pregnancy is the first 6 days of delay of the next menstruation. From conception is 3 week. Many women are confused because of the difference in numbers. In fact, everything is simple. In medicine, it is customary to calculate the period of pregnancy in obstetric weeks, they are counted from the first day of the last before the pregnancy of the month.
Thus, obstetric pregnancy began about two weeks before conception took place.
Approximately in the middle of the menstrual cycle, at the time of ovulation or a day after it, the meeting of the egg cell and the sperm cell took place. This day is the beginning of the embryonic period. Since the time of onset of ovulation may vary, it is more convenient to count the period of gestation from the first day of the last menstruation. If there is 4-5 obstetric week, it means that the most suitable time has come to reliably verify that there is a pregnancy.
How does the embryo develop?
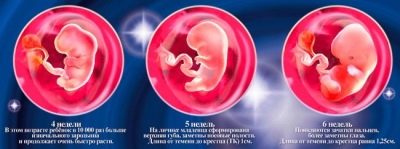
More recently, the baby was just a few cells that were constantly divided, and by now they have become a spherical blastocyst, which, 8 days after conception, has sunk into the uterus and entrenched there. Now, almost two weeks after the implantation, the baby looks like a cylinder about 1.5-2 mm long. It is on the fifth obstetric week that it is officially called the embryo., since the embryonic period of development begins.
Prior to this, the baby went through the germinal stage of development, then for 40 hours was in the implantation stage. All this time, the embryo could not be called an embryo, because in fact it was not yet. That stage, which starts for him this week, is the most responsible and important for the entire pregnancy.
Up to 9 weeks, when the embryonic period ends and the fetal (fetal) period begins, internal organs and systems will be actively formed, the first impulses of the nervous system will be debugged. Any harmful effects of teratogenic properties can cause mutations, gross anomalies and malformations, fetal death.
This week, the child lays the airway. The first will begin to develop the trachea, lungs and bronchi begin to form only after a couple of weeks. At 5 weeks after conception, the formation of the neural tube continues.How well this process will proceed depends on how the baby's head and spinal cord are formed, how its central nervous system will work. This week the neural tube closes, closes.
In 5 obstetric weeks, that is, in the very next few days, the baby will have sexual identification - the gonoblasts will begin to be laid in the yolk sac - the primary germ cells, which later become either sperm cells if the boy is conceived, or the eggs, if in the womb “settled " girl. At the cellular level these days, the digestive organs and the urinary system are being laid.
Nothing humanoid in the image of the embryo yet. It looks like a tadpole with an oval head germ, a protrusion where handles will soon appear. However, already at such an early date, a tiny heart appears in the embryo. As long as it has only two atria, it will divide into 4 chambers a bit later. At the end of this embryonic week, the heart begins to beat and soon it can be seen as a small flicker, and a little later you can hear it on the sensitive ultrasound machine.
To better imagine the size of the crumbs, you need to remember what a small rice grain looks like. By the end of the 5th obstetric week, embryo growth will be close to 4 mm. This baby is already demanding respect for himself and it is on the fifth week that he begins to “seek” a certain freedom and independence, self-expression.
It is separated from the embryonic structures (chorion, amnion and yolk sac). Now a young placenta will begin to form, to which, by the end of the first trimester, the embryonic structures will fully transfer their responsibilities for hormone production, protection, and nutrition to the fetus.
The development of a tiny embryo proceeds at a very fast pace: both externally and internally, the baby changes every day. Never in a person’s life is development and growth so rapid and intense as in the embryonic period of its development.
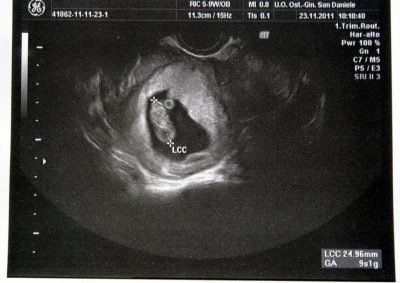
Ultrasound
To see the embryo on ultrasound during the fifth week is not always possible. The crumb is too small, not every scanner is able to identify it. But at the end of the week, at exactly 5 obstetric weeks, the chances that the baby is visualized are significantly increased.
Do not assume that the ultrasound scan will allow to consider the baby himself. At this time, at best, pregnancy is defined as an echo-negative liquid formation, which is a fertilized egg. Its average internal diameter is now about 4-5 mm. If ovulation was late, then the fertilized egg will have a smaller SVD, and it will probably not be possible to see it at all on an ultrasound scan this week.
In addition to size, the doctor must pay attention to the contours and outlines of the ovum. Normally, they should be smooth and clear. If the embryo is not yet visible, it is too early to sound the alarm.
A woman is given a second ultrasound after about a week.
Pregnancy is indicated by endometrial thickening, changes in the ovaries. The size of the yellow body in the normal range from 19 to 29 mm, the size of the yolk sac at this period is less than 5 mm. The yolk sac may also not be detected in the fifth week due to its small size, but after 7 days it will definitely be visualized if the pregnancy is proceeding normally.
Ultrasound examination this week is considered premature, since the risk of obtaining a false negative result is very high: they will not see the pregnancy, although it does. To save your nerves, women who definitely want to obtain documentary evidence of their pregnancy should wait about a week, at the 5-6 obstetric week, the diagnosis with the help of ultrasound does not cause any difficulties.
If the woman had no history of miscarriages and the pregnancy occurred naturally, and not with IVF, there is no need for an ultrasound scan. And although the harm from ultrasound exposure to the fetus has not been proven, no one has yet managed to prove harmlessness.
Experts recommend to go to such a diagnosis only as directed by the attending physician.
What does the future mother feel?
Some women do not feel anything unusual right now. But most of them say that their state of health has changed - rapid fatigability has appeared, I want to sleep and eat. There are also women who, at such an early date, begin to feel toxicosis - they are sick in the morning, sickened by the previously pleasant smell of her husband's cologne. Feelings at the physical level may resemble premenstrual syndrome - slightly pulls the lower back, stomach, as before menstruation.
Since the processes inside the female body are very intense and require a lot of energy, most pregnant women at week 5 say that they want to sleep more and move less. "Fads" can begin now. As a rule, they relate to changes in taste preferences - I want salted cucumbers, chocolate, herring with jam, tomatoes with sugar, etc.
To explain why such strange addictions arise, medicine cannot thoroughly, but there is a version that all this signals the body about the lack of certain substances necessary to ensure the growth of the embryo and changes in the woman’s body.
Changes in the body of a woman
An objective change at this time is a delay that goes back several days. Externally, the pregnancy is not manifested. But inside a woman there are numerous and very complex processes that should prepare her body for long-term fetal bearing and childbirth. Some women already on this period are beginning to darken nipple halos.
The breasts themselves increase insignificantly in size, a feeling of "fullness" appears, the fullness of the mammary glands, touching the nipples can cause pain, their sensitivity increases. The release of colostrum at obstetric week 5 is more peculiar to multiparous. Those who become pregnant with their first child may not have these symptoms.
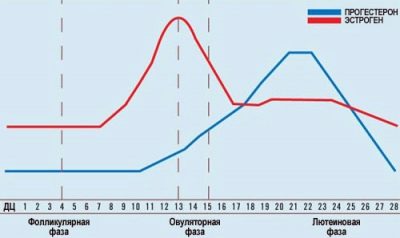
All other changes in the female body occur due to changes in hormonal levels. From the first minutes after conception, the hormone progesterone is produced in large quantities, which is necessary so that the uterus muscles do not stiffen, relaxed, and also so that the maternal immunity does not destroy the embryo: the hormone decreases the immunity ability baby's chances of survival increase.
The development of progesterone contributes to the hormone hCG. It is produced by chorionic membranes and enters the blood and urine of the expectant mother, growing every two days. By week 5, obstetric estimates show that the level of hCG becomes sufficient to diagnose pregnancy with rapid tests. Estrogens, female sex hormones, also support these two most important hormones for pregnancy.
Against the background of such a massive hormonal attack, the mood and psychological state of the future mother are usually the first to change. Already, a woman can pay attention to the fact that she has become more anxious, tearful, sensitive, sentimental.
Under the action of the hormone progesterone, digestion can be disturbed: heartburn will occur or diarrhea will begin. Some women emphasize that they have disturbed sleep, they hardly fall asleep, they feel overwhelmed.
Progesterone increases appetite. The uterus begins to round, before conception, it was more pear-shaped. This week, there will be a slight increase in the female reproductive organ in volume. This may cause small pulling back pain. Vaginal discharge may also increase.
Progesterone retains water in the tissues, this causes increased secretion. Many women feel increased salivation, for example, in a dream.
The same property of progesterone causes the appearance of physiological rhinitis of pregnant women - many in the 5th week have a runny nose without any other symptoms of a cold or ARVI. Hormonal "storm" in the female body is often the cause of fever in the evenings. The woman feels light chills, the temperature rises to 37.0 degrees or slightly higher. Many are starting to worry - are they sick? These symptoms have nothing to do with the disease. Usually in the morning the temperature is gone.
But the basal temperature, which some women continue to change in the fifth obstetric week, steadily keeps on subfebrile values - progesterone, as long as its level is sufficient to maintain pregnancy, does not allow it to drop.
Possible problems
The very beginning of pregnancy is not only joy due to the fact that “everything has finally worked out”, but also the likelihood of the emergence of various problems that a woman should know about. Here are just a few of them.
Biochemical pregnancy
Medicine claims that about 70% of women at least once in their lives have suffered a pregnancy, which was not even suspected, the so-called biochemical pregnancy. Any woman theoretically can face her this particular fifth week according to obstetric calculations. If on the first or second day of delay a particularly impatient expectant mother makes a test or gives a blood test, then they confirm the pregnancy. The test shows a distinct second strip, the level of hCG in the blood is determined, corresponding to the period.
But after a day or two this month, it can begin monthly. This phenomenon is called biochemical pregnancy. In fact, the following happens: the egg is fertilized, the implantation took place, but for some reason, almost immediately after implantation, the embryo is rejected, detached, and its death.
The hormone hCG has time to develop in certain quantities, it is this concentration that is displayed when performing a blood test. A week later, the fetus comes out, and it looks like regular periods, only slightly delayed and slightly more abundant than usual.
The reasons for which the baby can stop development after implantation are numerous. Often the root of the problem lies in the immune processes, sometimes in chromosomal abnormalities that have arisen during the merger of the sperm with the egg. Often, biochemical pregnancy occurs in women with inflammatory diseases of the reproductive organs, as well as endocrine disorders. But the true causes of this phenomenon have not been studied.
Biochemical pregnancy is not considered a miscarriage, it does not affect the subsequent pregnancy and childbearing. Often the fact of such pregnancy generally goes unnoticed, and the woman thinks that her period simply came with a slight delay. Symptoms and signs characteristic of pregnancy normal, usually not.
The only way to establish BHB (short name for biochemical pregnancy) is a blood test for hCG.
Anembrionia
This term refers to the pathology of pregnancy, in which there is no embryo inside the ovum. The egg itself usually grows, and the dynamics of its growth can be well traced by ultrasound. On such a short period, anembryonia is often mistaken, and the reason lies in late ovulation. According to obstetric calculations, a woman is in her fifth week, but due to late ovulation and implantation, the fertilized egg is still small, and the embryo has tiny dimensions.
True anembryonia may be the result of an adverse effect on the fetus - radiation, medications, poisons, unhealthy genetics. Usually the cause can not be established. The fifth week is too short a time for such a diagnosis. If now this assumption has been heard by the ultrasound doctor, it is necessary to calm down, wait 7-10 days and again visit the ultrasound diagnosis room.
During this week, you can do a blood count 2 times for HCG. With progressive pregnancy, the level of the hormone will increase rapidly.
At 6-7 weeks of pregnancy, the embryo on the ultrasound should be clearly visible, regardless of the timing of the onset of ovulation. If anembrionia is confirmed, the woman will be shown curettage of the uterus or a medical abortion.
Fading Pregnancy
Stay in development, stop the progress of pregnancy in the embryonic period can at any time, and the reasons for this set. This includes inflammatory and infectious diseases in a woman, her bad habits, stress, worries, excessive physical exertion. However, not everything depends on the most pregnant. If the embryo has anomalies due to chromosomal abnormalities, in many cases its further development becomes simply impossible.
Sometimes the cause of fading lies in paternal sperm - if the morphology of the male germ cells is violated (teratozoospermia), conception is difficult, but it is possible, but the risk is higher than the formation of the wrong set of genetic fetuses.
At week 5, it is difficult to recognize such a non-developing pregnancy, but it is possible. If a woman suddenly had signs of toxemia that were already present, if her chest suddenly stopped hurting, her general condition changed, and nothing indicates a probable pregnancy, with a great deal of truth you can say that fetus may stop. More informative will be a blood test for hCG. After fetal fetal death, hormone levels begin to decline.
And two tests over the course of a week will be quite enough for the doctor to be suspicious and send a woman to an ultrasound.
After about 2-3 weeks, a dead embryo, if a miscarriage has not occurred earlier, may gradually begin to be rejected by the maternal organism. Appear brown spotting, pulling pain in the lower abdomen and lower back. When the diagnosis is confirmed, the woman is subjected to surgical curettage and anti-inflammatory antibiotic therapy is prescribed or a medical abortion is performed.
It is advisable to examine embryo tissue samples in the genetic laboratory in order to try to determine whether certain chromosomal abnormalities and mutations of genes have caused the stopping in its development. This information is necessary for the further planning of the next pregnancy.
Ectopic pregnancy
As the name suggests, such a pregnancy is connected with the anchoring of the fetus not in the uterus, but outside its cavity, for example, in the fallopian tube or in the cervix. The causes of this phenomenon can also lie in a variety of pathologies of the female reproductive system, hormonal disorders, and infectious diseases. At week 5, it is not always possible to establish an ectopic pregnancy.
The main sign of uterine pregnancy is the presence of the ovum in the uterus. To see him at week 5, as we found out, is not always possible, and this still does not indicate the obligatory presence of pathology.
The only way to suspect such an abnormal pregnancy at such a short time is a blood test for hCG. The level of human chorionic gonadotropin in the body with ectopic embryo attachment is always significantly below the norm, the test strip from the pharmacy can generally show a negative result or a weak unexpressed second strip even several days after the delay.
Based on a blood test, no diagnosis is made, and doctors will prefer to wait another week to make sure that there is no ovum in the uterus. Symptoms at week 5 may not be present, but it is possible that pain may already appear in the lower abdomen, on the right or on the left, which depends on the specific part of the fertilized egg. At week 5, pain may occur in women in whom the embryo “settled” in the narrowest part of the fallopian tube.
If the fetus is located and develops in the wide part of the tube, then the symptoms will not start before 8 weeks, and if the embryo is fixed closer to the ovary or in the abdominal part, then the first unpleasant symptoms usually appear by the end of the 6th week of pregnancy. In addition to pain, there may be a brown discharge with streaks of blood.
Unfortunately, doctors cannot do anything. Ectopic pregnancy is doomed to interrupt. The task of doctors is to do this as early as possible, to prevent rupture of the fallopian tube or cervix. After such a pregnancy, if the tubes, the ovaries could be kept, a new pregnancy is quite possible after a course of treatment.
If the pregnancy is found in the cervix, the predictions are less optimistic. Typically, such a pathology (by the way, rarely occurring) requires surgeons to completely remove the uterus.
Early toxicosis
Early toxicosis is not such a rare occurrence. It all depends on how it flows. Moderate nausea and even vomiting in the morning is a normal variant, but if the vomiting is exhausting, persistent, it repeats several times a day, the woman cannot eat, then this condition is fraught with dehydration and threatened miscarriage.
Strong early toxicosis needs medical attention. Vitamin preparations are administered to the woman to compensate for the growing embryo's lack of nutrients and minerals in the mother's blood. Toxicosis usually retreats closer to week 12-13.
The reasons for which some women have toxicosis, while others have no hint of nausea and dizziness, medicine is not known for certain. Experts tend to believe that toxicosis is caused by the individual characteristics of a woman’s immune system, as well as by the changed hormonal background.
Diagnostics
The main symptom that cannot remain unnoticed by a woman at the fifth obstetric week is the absence of a regular menstruation on the appointed day. This means that it is now possible and necessary to find out the reasons for the delay. On this period, you can use different methods for diagnosis, with the exception of ultrasoundwhich, as a rule, cannot yet answer with confidence the question whether there is a pregnancy.
The hormone hCG, which began to be produced immediately after implantation, this week in the blood rises at least 60 times compared with its norm for non-pregnant. A blood test from the very first day of the delay will leave no doubt that the woman is now pregnant. The rate of hCG for this week is from 300 to 5000 IU / liter.
The concentration of chorionic hormone in the urine also exceeded the sensitivity thresholds of rapid tests, which can be easily obtained at any pharmacy. If the threshold of sensitivity of the test is on average from 20 to 30 units per milliliter, then on the first day of delay the test will show the second strip.
Which of the ways to use to diagnose pregnancy at this time is only for the woman herself. The blood test has its advantages - it allows not only to establish a pregnancy, but also to make sure that it develops normally, if the level of the hormone corresponds to the term.
If the concentration of chorionic gonadotropic hormone is above the norm, it can even be assumed that the woman in the womb has not one, but two embryos.
A decrease in the amount of hCG in the blood may indicate a threatened miscarriage in the early period. Home rapid test, even the most expensive, for example, electronic, will not give so much useful information. He will only show the fact of pregnancy without details. But it is easier to carry out, it does not require special training. Any woman can easily cope with the task.
In fairness, we note that the accuracy of the home test is lower than the accuracy of laboratory blood tests. Test strips are more often defective, give false positive and false negative results.
If there is the first week from the beginning of the delay (this is the 5th obstetric week), and the test is negative, then you should donate blood for hCG and visit the doctor with this result.
Analyzes and surveys
On the pages of women's forums there are serious disputes about when to contact the antenatal clinic for registration. The answer can be only one - the sooner the better. Early registration will reveal possible pathologies at an earlier stage, for example, detect ectopic pregnancy at the stage when it is easy to perform laparoscopic surgery and preserve reproductive women's health, and not when the growing fetus tears the fallopian tube to shreds and to save the woman’s life will have to remove it completely.
No one, of course, forces a woman to go to the doctor immediately after the home test, which showed two cherished strips. But waiting for the pregnancy to “step over” 8-10 weeks is also not worth it. If there is a desire, then this question can be closed once and for all by visiting the gynecologist at the end of the 5th obstetric week of pregnancy.
It is advisable to have the results of the blood test for hCG with you so that the specialist has no doubts about the fact of pregnancyAfter all, manual research on this period does not always show a significant increase in the size of the uterus.
If such a decision is made, the woman should know that she will be well prepared to prepare for the first prenatal screening, which runs from 10-11 to 13 weeks of pregnancy, inclusive. The training will consist in the slow passing of all the analyzes that were required for registration, as well as visits to doctors of other specialties, which is recommended in the first trimester.
At the first visit to the doctor, the card of the pregnant woman and the parturient woman is filled in, a small copy of it is issued - an exchange card, which is given to the woman. Now this is her main document, which you should always carry with you, especially at your next consultation. The results of all tests, ultrasound will be recorded in the exchange card. It is with this card that the woman will go to the maternity hospital when the due date for delivery.
The tests that will be prescribed at the first stage are numerous. These are general blood and urine tests, and a vaginal smear on the microflora, and extensive biochemical blood tests. You will have to donate blood for HIV and syphilis, hepatitis, for TORCH infections (rubella, cytomegalovirus, herpes, toxoplasmosis). A woman is obliged to confirm her blood type and Rh factor.
If she has a negative Rh, her partner will also have to come to the consultation in order to donate blood for the group and Rh.
At the very beginning of pregnancy, blood tests for hormone levels, as well as ultrasound of the pelvic organs with the threat of termination of pregnancy, can be assigned according to individual indicators.
Recommendations
In spite of the fact that you have just learned about pregnancy, the way of life should be necessarily corrected for future imminent changes. The child will not, he already is, and right now the baby needs maternal protection and optimal conditions for its development. Simple recommendations will help to help the embryo develop properly.
Vitamins
Already, the embryo and the maternal organism begin to feel the need for certain substances. This week, given that the nervous system of the fetus is actively being formed, it is imperative to start taking folic acid. Optimal to take it before conception, but if this did not happen or the pregnancy was not originally included in the couple’s ambulance plans, now is the time to start supplying yourself and the baby with this useful substance.
In regions where there is no sea and sun, women are advised to take iodine supplements in addition. But vitamin complexes, which are widely publicized and quite expensive, do not be in a hurry to buy.It is worth waiting for the results of the biochemical analysis of blood, which also shows how great a woman’s need is in certain minerals and vitamins.
This is another big plus of early registration - there is an opportunity to choose an individual, necessary for this future mother drug containing multivitamins and minerals.
Sometimes vitamins and mineral supplements are recommended to be taken not as part of a complex, but separately.
Sex
Having sex at obstetric week 5 is possible. The child's intimate life of the parents does not harm, if the woman has no obvious contraindications. If sexual activity is not yet desirable, the doctor will inform the woman of this, given her obstetric history. For contraindications include habitual miscarriages in the early stages, atypical for this period of discharge or pain in the abdomen.
After IVF should be especially careful, including in matters of active sexual life, because the uterus at the time of orgasm comes in tone, which can provoke the detachment of the ovum.
If there are no contraindications, then sex will only benefit the woman. They improve her mood, make his differences less noticeable, instill a sense of their own need and importance for this man, improve the microclimate in the family and relations between partners.
Now normal relationships are more important than ever, because the stresses caused by conflicts in the family, according to statistics, occupy one of the first places among the causes of spontaneous abortion at an early period.
Nutrition
As soon as the test showed two strips, a woman should think about proper nutrition. Despite the insistent demands of the body who wants herring with jam or honey and bacon, it is worth taking the issue seriously and reconsidering your diet.
Proper nutrition will help keep under control the weekly weight gain, which has already begun, and will not allow a woman to gain extra pounds, which can significantly complicate the last months of carrying a baby and the upcoming birth.
Balanced fractional nutrition will reduce the effects of progesterone on digestion - will reduce flatulence, bloating, prevent heartburn, constipation and diarrhea. Properly selected products will provide the female body and the rapidly growing body of the crumbs with everything necessary.
First of all, it is necessary to refuse fried, fat, excessively salty and sweet. It is important to eat fresh vegetables and fruits, lean meat, fish, dairy products.
You need to eat at least 5-6 times a day, the last meal - 3 hours before bedtime. Fluids should drink at least one and a half liters - now the embryo has a need not only for nutrients and vitamins, but also for water. A woman “in position”, even in the earliest terms, is prohibited from carbonated drinks, store juices in packs, baking, condensed milk, chocolate. The amount of salt should be reduced to 5 grams per day.so as not to create prerequisites for the appearance of edema and the development of preeclampsia dangerous for the mother and fetus.
Medicines
Quite often, in the first weeks of pregnancy, a woman has exacerbated chronic diseases, because the load on all organs increases tenfold. Reduced immunity in the early period can cause infection with a viral or other infection. Doctors say that diseases at the beginning of gestation are not as dangerous as the uncontrolled intake of medicines that are not agreed with the doctor.
Many drugs have a teratogenic effect, they are dangerous for the emerging embryo. The most dangerous are antibiotics, immunostimulants, antidepressants, antiepileptic drugs, many painkillers.
Therefore, when a cough appears, if a tooth, head, stomach or kidney hurts, you should not take drugs that have always helped in these situations, no matter how great the temptation.The pills that the woman took before pregnancy can cause serious harm in the early stages of pregnancy.
The best solution is to deal with the pain to the doctor. He will be able to pick up drugs that can be taken by pregnant women, and if there are none, he will tell you a couple of prescriptions from the field of alternative medicine that will help a woman relieve her condition. The less mom before the 12th week of pregnancy will be eaten tablets and capsules, the fewer injections will be made, the better for the fetus.
Working conditions
The fifth week should be a turning point and in the working schedule of the woman. If her work is connected with shift work at night, then now is the time to get a certificate in the antenatal clinic and show it to the superiors so that the work schedule will be changed exclusively to day time.
Night sleep is important for any person, because it is precisely at night that certain hormones important for health, protein compounds, and enzymes are synthesized. For a pregnant night sleep is doubly important.
The labor code of the Russian Federation allows expectant mothers to receive, on demand, a time-limited and strictly limited working day, safe and harmless working conditions, and a lunch break. Many are afraid to ask for their leadership, because they are afraid of dismissal. It is impossible to dismiss a pregnant woman by law, so there’s absolutely nothing to worry about.
Women in the early stages are contraindicated in work in paint shops, in shops with strong noise and vibration, in industries related to electromagnetic or radiation exposure. A woman has the right to refuse long trips, from overtime work. For early registration, a small amount of up to 600 rubles is added to maternity payments.
Lifestyle
Two strips on the test - not a reason to sit on the sofa and sit there all 9 months. At this time, a woman should continue to lead her usual lifestyle. If she was involved in sports, you should slightly reduce physical activity., but to abandon them is absolutely not necessary, of course, if the doctor permits.
If earlier a woman didn’t play sports, it’s time to start doing light exercises in the mornings, and in the evenings to go to the swimming pool, swim, do water aerobics, and make evening walks in the open air before going to bed. Such a lifestyle will not be associated with excessive loads, but will not allow to conduct a hypodynamic lifestyle, fraught with obesity, difficult childbirth, a long recovery postpartum period.
Alcohol and nicotine
Many women are interested in how alcohol and nicotine will affect a child, which a woman may have taken before she learned that she is pregnant. If alcohol does not imply chronic alcoholism, systematic intake of strong alcoholic beverages in large quantities, then there is no harm to the embryo. The main thing now is to refrain and not allow intake of strong drinks.
Nicotine is a bit more complicated. If we are talking about a chronic smoker who has this bad habit for 10 years or more, then you should consult with your doctor - in some cases, a complete rejection of cigarettes provokes a miscarriage, as it leads to withdrawal syndrome associated with changes in blood pressure, hormonal changes .
Such pregnant women are sometimes offered as an exception cigarettes with a lower nicotine content and a reduction in the number of cigarettes smoked to 1-2 per day.
If everything is not so neglected, then A woman is recommended to quit smoking immediately after the discovery of two stripes on the rapid test. Nicotine is very dangerous in the period when the nervous system is formed, as well as the baby’s heart and blood vessels.
Reviews
Many women at this time are actively discussing the reaction of their husbands to the news that soon there will be an addition to the family. Men do not always react to this with sincere joy, and therefore there are plenty of reasons for worrying future mothers now.Many are trying to sign up for an ultrasound on this week to be sure of their imminent motherhood.
A lot of questions and doubts this week are the tests and their results. The most accurate, but expensive, women are almost unanimously considered electronic tests, which, according to the concentration of hCG in the urine, indicate the expected period in weeks. Those who have already begun toxemia are perplexed, because in general opinion it is too early for nausea, but medicine claims that this is also a variant of the norm.
About what happens in the 5th week of pregnancy, see the next video.