IVF short protocol by day: scheme and description
When it is impossible to get pregnant, many women have to resort to assisted reproductive technologies. At the end of the preparatory stage, when the woman passes all the necessary tests, the fertility specialist will choose the optimal protocol for her - her personal infertility treatment regimen. Two types of schemes are widely used in Russia - the long and short protocols. On the short we will tell in this article. Let us consider in detail its pros and cons, the advantages, the description and the detailed scheme by day.
What it is?
The short IVF protocol is considered more benign than the long one, since with it the hormonal stimulation of the ovaries does not have that span and scale, as with any subtype of a long protocol. Independently, a woman cannot choose the type and scheme of treatment; her reproductive doctor should decide on a specific protocol, who, when choosing, will rely on the results of tests, on the features of the endocrine system of a particular patient, on her age and causes of childlessness.
If the doctor recommends a short IVF protocol, it means that he has every reason to do so.
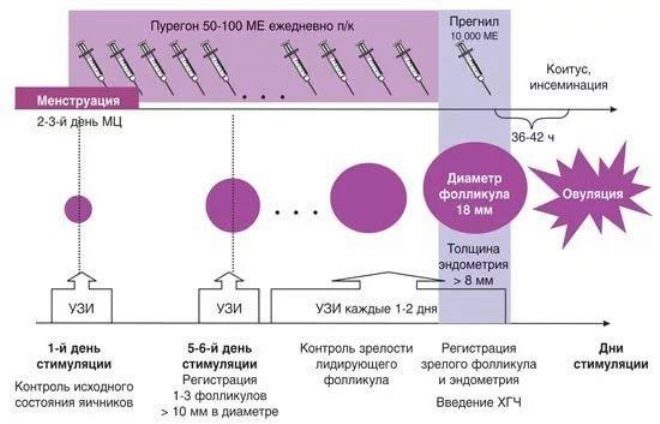
A short protocol always starts on the 3rd day of the menstrual cycle and lasts no more than 28-36 days, while the hormonal stimulation itself takes no more than 10-16 days. The ultrashort protocol lasts no more than 26-30 days, while the hormonal stimulation stage takes no more than 7-10 days. Compare yourself: a long protocol sometimes lasts up to one and a half months, and in super-long - up to six months.
It turns out that the inevitable aggressive effect of hormones on the body of the fair sex in the protocol of the short type is reduced to the minimum values, which makes the protocol easier for the patient to feel and minimizes possible complications and consequences.
Advantages and disadvantages
The main advantage of the scheme for the short type is a smaller amount of hormonal drugs that women will have to take in the first phase of the menstrual cycle. This not only saves women's health, but also significantly reduces the cost of IVF, because almost half of the total cost of the protocol consists of the cost of expensive hormonal drugs.
Short protocols, according to the established practice, are considered the most preferable for women with normal or large ovarian reserve, with oocytes of satisfactory or good quality. If the oocytes are weak and non-viable, if they cannot be fertilized even in the laboratory, a long protocol is more suitable.
Often, short protocols are recommended for women after the age of 35-37 years old, but there is one important condition - all the functions of their sex glands (ovaries) should be preserved by this age in full. Quite often, a change of protocol from a long but unsuccessful to a short one leads to the desired result - pregnancy begins.
The undoubted advantage of the short type protocol is the relatively low risk of developing such an unpleasant and even dangerous complication as ovarian hyperstimulation syndrome. This IVF regimen is more easily tolerated by patients.
Among the shortcomings that are mandatory for each treatment regimen, for the short type protocols, two aspects deserve special attention:
- the probability of arbitrary ovulation, which will not give the opportunity to get the oocytes and the protocol will have to be interrupted and repeated in 2-3 months;
- short hormonal stimulation does not allow to obtain a large number of oocytes, so there is no possibility of choosing the best quality cells. Usually, all that is received is subject to fertilization. Because of this, the risk of replanting low-quality embryos increases. The success rate of IVF in the short protocol is always lower than in the long one.
Stages of the treatment cycle
The short protocol is less like a violent interference with the work of the female body. It is fully consistent with its biological nature and flows in accordance with the natural cycle.
After the onset of menstruation, the woman should come to the doctor and be assigned to the beginning of the protocol. On the 3rd day of the cycle, hormonal preparations are started. When the follicles mature, ovulation is stimulated with other hormones. After that, after 36 hours, the woman is punctured the follicles and the oocytes mature and ready for fertilization are taken.
At the next stage, the eggs are fertilized with sperm of a spouse, partner or donor (depending on IVF conditions). After a few days in the nutrient solution and after assessing the quality of the embryos, the embryologist carries out the transfer of the embryos to the uterus.
If the protocol is successful, the embryo (or several at once) is implanted into the endometrium of the uterus, and pregnancy begins.
On the 3rd day of the menstrual cycle, a woman takes medications that partially block the work of the pituitary gland by agonists (for example, Dexamethasone). At the same time, stimulation with follicle-stimulating preparations and menopausal gonadotropins (Meriofert) is carried out. After puncture of the follicles, the woman begins to take progesterone drugs in order to maintain the second phase of the cycle and, under favorable conditions, promote implantation and fetal bearing.
Scheme by days
There are three main types of short protocols, which are slightly different mainly selected hormonal drugs. It:
- agonist hormone protocol;
- protocol with hormone antagonist drugs;
- Ultrashort antagonist protocol.
When the protocol with agonists is stimulated with Dexametozon or other hormones that are related to menopausal gonadotropins, or with GnGRH (Dekapeptil) agonists, it starts on the 2nd day of the menstrual cycle and ends on the 5th day.
On the 14th day of the cycle, the follicles are punctured. A step-by-step description of the procedure will help the woman not to be afraid of collecting eggs: everything passes under anesthesia, lasts no more than 15 minutes. When the patient falls asleep after the introduction of intravenous anesthesia, the doctors with a long needle, under ultrasound control, puncture the posterior wall of the vagina, reach the ovaries and “pull” through a needle into special sterile containers the follicular fluid with the oocytes present in it. This procedure ends.
When a woman wakes up, she is prescribed progesterone drugs to maintain the second phase and is allowed to go home until the day of embryo transfer.
How women’s well-being will change during the short protocol, the question is ambiguous. Some do not have any significant changes. Others tolerate it more difficult, it all depends on individual sensitivity. From the 3rd day of the cycle, when GGNG agonists are stimulated, as well as with ovulation stimulating drugs (Puregon, Gonal), feelings of bloating in the stomach, hot flushes, slight nausea and episodic headaches may appear.
Many women note a highly unstable psychological and emotional state in which tears are replaced by anxiety, and laughter - by a depressive state. This is a side effect of agonists and antagonists. Gradually, this will pass, you just need to be patient.
Every two days a woman will need to visit the clinic and do an ultrasound scan so that the doctor can monitor the maturation process of the follicular vesicles on the sex glands. With an abnormal reaction of the ovaries to hormones, the dose and the multiplicity of the drug can be changed by the doctor at his discretion. Stimulation by hormones lasts no more than two weeks.
Features of
Almost all medicines that will be prescribed by a doctor to stimulate the ovaries are available in injectable form. This means that a woman will have to do injections. It is inconvenient to visit the clinic every day at the same time, so doctors are allowed to make subcutaneous and intramuscular injections at home.
In this case, be sure to bear in mind that skipping the next injection is not allowed. It can lead to a breakdown of the entire treatment course and note the efforts of doctors to zero.
Subcutaneous injections are introduced into the abdomen, intramuscular injections are made in the standard place for such cases - the buttocks. Hormone therapy differs from treatment with other medicines in that it is necessary to inject the medication at regular intervals of time daily, increasing or decreasing the dosage is prohibited. Make adjustments to the short scheme (yes, in the long too) can only the attending physician.
With a normally flowing short-type protocol, the follicles on the ovaries should increase by an average of two millimeters each day, and the thickness of the endometrium should increase by at least one millimeter per day. When growth is more intense, the doctor may reduce the dose of medication. If growth is insufficient, the dose may be increased.
As soon as the follicles (at least three) reach 17-22 mm, the doctor prescribes a single injection of any drug that is considered an ovulation trigger. Under the action of such hormones, the egg cells detach from the inner walls of the follicular vesicles and remain in the follicular fluid. They will be easy to “get” at puncture.
Reviews
In their responses, women often cite examples of their own short protocol outlines showing the drugs and dosage. Those who are just entering into the protocol and turning to the all-knowing Internet for opinions and advice should in no case be guided by other protocols, since their own treatment regimens may differ, as drugs and dosage differ.
Many women recommend to follow a protein diet and drink enough liquid to avoid hyperstimulation of the sex glands, which still exists with a short protocol.
Proper nutrition even before entering into the protocol, taking vitamins will help not only easier to go through the stimulation stage, but will also help improve the quality of the eggs.
Short protocols, unfortunately, are less successful, as evidenced by most reviews of women who received such treatment. However, those who did not despair and after three months made a second attempt, quite often say that the likelihood of getting pregnant increases with subsequent short protocols.
After a short protocol, even if it is not completed successfully, the reproductive system is “restarted”, and approximately a quarter of couples with endocrine or implicit causes of infertility can conceive a child in a completely natural way.
The fact that such a short protocol IVF, see the following video.