What anesthesia is better to choose for caesarean section?
Cesarean section is performed exclusively under anesthesia, as it is abdominal. Surgical anesthesia is discussed in advance if the surgery is planned. And a woman can choose this or that type of anesthesia, but not always. Sometimes it must be done only by a doctor. In this article we will talk about what choices exist, how they differ, what are their advantages and disadvantages, and also describe the situations in which a woman cannot make an independent choice.
What is considered when choosing?
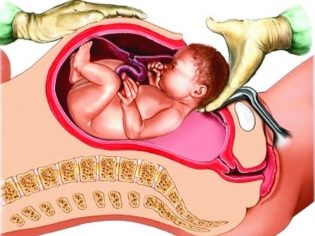
The operation involves dissection of the anterior abdominal wall, the uterus, removal of the child and manual separation of the placenta, after which the internal sutures are first applied to the uterus, and then external to the incision in the peritoneum. Surgical intervention lasts from 20 minutes to an hour (in particularly difficult and difficult cases), and therefore under local surface anesthesia, such an operation cannot be performed.
Today, during cesarean section, two types are used. anesthesia - epidural (and, as a species, spinal or spinal) and general anesthesia. In case of emergency caesarean section, which is carried out to save the life of the child and the mother, if something goes wrong in natural childbirth, general anesthesia is usually applied by default. The question of choosing a method of anesthesia for caesarean section is usually decided in advance only when the operation is planned in advance.
In this case, doctors evaluate a lot of factors. First of all, the state of the pregnant woman and the fetus, the possible influence of the drugs that are used for pain relief, on the child and the mother. It is necessary to take into account certain contraindications and indications for different types of anesthesia. Regional (epidural) anesthesia has contraindications, whereas there are no contraindications for general anesthesia.
Epidural Anesthesia
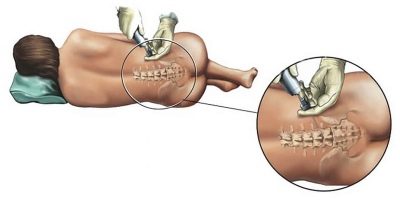
In this way, up to 95% of all cesarean section operations in Russian maternity homes are anesthetized today. The essence of the method lies in the fact that the introduction of the drug, which leads to loss of pain sensitivity in the lower body, is done through a thin catheter inserted into the epidural space of the spine.
As a result of this injection, the transmission of nerve impulses to the brain via the spinal canal is blocked. When such a gap arises in the chain of the central nervous system, the brain simply does not perceive and does not associate the ongoing violation of the integrity of the tissues during the operation as a pretext for activating the pain center.
The scope of such anesthesia is wide enough, but with natural childbirth to relieve pain and caesarean section, such anesthesia is considered less dangerous than with anesthesia of the cervical spine or hands for operations on the upper part of the body.
As a rule, anesthesiologists inject special, thoroughly cleaned solutions, which are originally intended exclusively for such an application. To relieve pain in natural childbirth, lidocaine and ropivacaine can be administered.But for caesarean section such anesthesia will not be enough. Simultaneously with lidocaine, a certain amount of opiates can be administered, for example, prozedol, morphine or buprenorphine. Ketamine is often used.
The dosage of substances is determined by the anesthesiologist, taking into account the health status, weight and age of the woman, but for spinal anesthesia opiates are always required less than with intravenous anesthesia, and the effect can be achieved over a longer period.
How do?
The woman lies on her side with her back bare, legs slightly stretched and shoulders forward. An anesthesiologist one of the existing methods determines exactly where you need to enter the catheter. To do this, usually use a syringe filled with air that is connected to the catheter. If the piston encounters significant resistance, then the catheter is in the ligamentous space. If resistance is suddenly lost, we can talk about the correct detection of the epidural space, where it is necessary to slowly introduce drugs.
The introduction is stepwise. This means that the doctor first enters the test dose. After three minutes, the condition is assessed, and if the first signs of anesthesia, loss of sensitivity, appear, the rest of the dosage for a specific woman is administered in several steps.
A woman may first ask the anesthesiologist, who will definitely meet her the day before the operation, the name of the drugs that are planned to be administered. But it is better not to ask about the dosage, since its calculation is extremely complicated and based on numerous factors.
The operation begins after a complete blockage of the lower body occurs. A screen is installed in front of the face of the woman so that she does not see the surgeons' manipulations. Throughout the whole operation, a woman in labor can communicate with doctors, see the main point - the first breath and the first cry of her baby.
After that, the doctors will start stitching, and the baby may well be left next to the mother for a few minutes so that she can admire the long-awaited crumb of plenty.
Advantages and disadvantages
Complications after such anesthesia are possible, but in practice they are found only in 1 case per 50,000 births. What could be unexpected and negative manifestations? It happens that the blockade of nerve endings does not occur, the sensitivity persists, and this, according to statistics, happens in one woman for 50 operations. In this case, the anesthesiologist urgently makes a decision on general anesthesia.
If a woman has problems with blood clotting, a hematoma may develop at the site of the catheter insertion. When inserting a needle, the anesthesiologist can accidentally puncture a solid spinal sheath, which is fraught with leakage of cerebrospinal fluid and subsequent problems with severe headaches.
Inaccurate movements of an inexperienced doctor may cause injury to the subarachnoid space, as well as the development of paralysis. Opponents of general anesthesia suggest that, with epidural anesthesia, the drugs administered do not have any effect on the child, in contrast to the total drug sleep, in which the woman in childbirth is immersed during general anesthesia. This is not true. Medications that are administered for the blockade of pain can cause a decrease in the heart rate of the baby, as well as a state of hypoxia or breathing problems in him after birth.
Many women in labor complain about back pain and numbness for quite a long time after surgery. It is officially considered that the time to exit from spinal anesthesia is a gap of about 2 hours. In practice, the output is longer.
The advantages of epidural analgesia include the stability of the heart and blood vessels of a woman throughout the operation. A significant disadvantage is that not all nerve receptors are blocked.A woman will not feel pain directly, but at times she will have to endure the discomfort.
Many women are wary of such anesthesia, because not even complications frighten, but the very need to be present during one's own surgery is psychologically difficult.
Often, women consider epidural and spinal anesthesia to be the same type. In fact, for the patient there is no difference, in both cases the drug is injected into the back. But with spinal cord injection, a deeper one, and therefore, sensitivity decreases more effectively.
If the question is a matter of principle, specify where the doctor plans to do anesthesia - in the epidural space of the spine or in the subarachnoid. Otherwise, everything will proceed in the same way.
General anesthesia
Previously, it was the only type of analgesia cesarean section. Now they resort to general anesthesia less and less. Officially, this is explained by the fact that general anesthesia harms the child and the woman. It is unofficially known that the cost of drugs for spinal or epidural anesthesia is lower, and therefore the Ministry of Health in Russia strongly recommends anesthesiologists to persuade women to choose regional anesthesia. This question is complex and ambiguous.
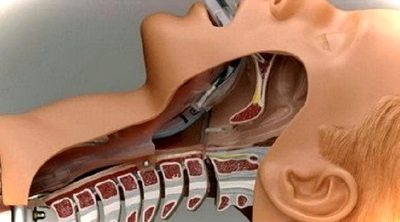
General anesthesia for surgery KS is usually used endotracheal. With him, the woman does not feel, hear or see, she sleeps quietly throughout the surgery, not worrying herself, or twitching with questions from the doctors who help her baby come to light.
How do?
Preparation for such anesthesia begins in advance. In the evening, on the eve of the day on which the operation is scheduled, premedication measures are taken - the woman needs to relax, sleep well, and therefore she is prescribed a dose of barbiturates or other serious sedatives before going to bed.
The next day, a dose of atropine is administered to the woman in the operating room in order to exclude cardiac arrest at the time of being in medication sleep. Analgesics administered intravenously. At this stage, the woman, not having time to be afraid of what is happening, falls asleep.
When she is already in a state of sleep, they will introduce a special tube into her trachea. Intubation is necessary to ensure pulmonary respiration. A tube through the lungs will deliver oxygen mixed with nitrogen, and sometimes narcotic fumes throughout the operation.
Sleep will be deep, the anesthesiologist throughout the intervention will monitor the condition of the woman, measure pressure, pulse, and other indicators. If necessary, the dose of injected support drugs will increase or decrease.
Shortly before the end of the operation, the anesthesiologist begins to reduce the doses of muscle relaxants and anesthetics, narcotic substances. When the doses are “zeroed out”, the process of smooth awakening begins. At this stage, the tube is removed from the trachea, since the ability to breathe independently, without an artificial respiration apparatus, is one of the first to return.
Advantages and disadvantages
Psychologically, general anesthesia is much more comfortable than regional anesthesia. A woman does not see what is happening and does not hear the conversations of doctors, who at times can plunge anyone into shock, and even about a patient lying on the operating table. A woman comes out of a state of relaxation and inhibition quite easily, but finally, only 3-4 days after anesthesia leave. The final solution is considered to be the complete cessation of the effect of the anesthesia performed at all levels of physiological and biochemical processes in the body.
A big plus is the complete absence of contraindications, that is, this method is used for all who require surgical intervention, without looking at possible negatively influencing factors. The quality of anesthesia is on top.
There will be no sensations - neither pleasant nor painful women will feel. Possible complications of endotracheal anesthesia include possible injuries of the larynx, tongue, teeth (at the time of insertion and withdrawal of the tube), laryngospasm, the development of an individual allergic reaction. Quite often, women after such anesthesia have a sore throat for several days, a dry cough is observed (which is especially painful with fresh stitches on the abdomen!).
If a woman decides to choose general anesthesia, she should understand that she will not meet with the child immediately. She will be able to see the baby only after a few hours, when she is transferred from the intensive care unit to which all operated women in labor are transferred to the postpartum hospital.
However, in some situations this issue is resolved on the spot - a woman can ask the operating team to show her the baby immediately after she comes to her senses. True, whether the newly made mother herself remembers this moment or not, no one will guarantee.
When the question is decided only by a doctor?
If a woman who has a planned caesarean section is set up for a certain type of anesthesia, she can report it to her doctor, who will give the information to the anesthesiologist. The woman signs an informed consent that she agrees to epidural anesthesia or writes a waiver of regional anesthesia.
Indicate the reasons for which the decision was made in favor of general anesthesia, the pregnant should not. She generally can not justify their decision even in a conversation with a doctor.
According to the law, in case of written refusal of the woman in labor from epidural or spinal anesthesia, general anesthesia is automatically used for her. There can be no second solution. But the reverse situation, when a woman would like to be conscious during the operation, can turn in different ways.
Epidural anesthesia has its own contraindications. And no matter how the woman pleads with the doctor to make her a corner in the back before the operation, the request will be denied if:
- previously there were injuries or spinal deformities;
- there are signs of inflammation in the area of the intended needle;
- the woman has low and low blood pressure;
- the woman has started bleeding or there is a suspicion of starting bleeding;
- there is a state of fetal hypoxia.
For women with such features is considered the best general anesthesia.
They will not ask the patient's opinion on the preferred type of anesthesia even if there is a loss of umbilical cord loops, if the woman has a systemic infection, if necessary, remove the uterus after the baby is removed (if indicated). Such mothers also performed only general anesthesia. Other options are not even considered.
Reviews
According to medical practitioners, general anesthesia is more preferable for them, since with her the woman in labor is completely relaxed, and, as the surgeons say, does not interfere with work. It is also technically easier for anaesthesiologists to perform general anesthesia than to risk trying to find the right place inside the spine. But the recommendations of the Ministry of Health cannot be ignored, therefore regional anesthesia is presented as optimal.
According to the patients, after general anesthesia, they come to life faster and softer. After epidural anesthesia, numbness in the extremities persists for a long time, which somewhat limits the recommended early physical activity. But the opportunity to see the baby at the time of birth, according to many moms, is worth it.
On the types and methods of anesthesia during surgery, see the following video.