Placenta thickness by week of pregnancy
During pregnancy, special attention is paid to the placenta. Much depends on her health: the child’s well-being and development, his life. When assessing the placenta, a parameter such as the thickness of the “children's place” is used. You will learn about what it should be at different periods of gestation, what the reasons can be, the consequences of deviations from the norms, after reading this article.
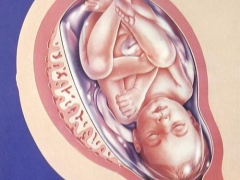
Structure and function
The placenta is a temporary organ, necessary only in the process of carrying a child. It provides a close relationship between the mother and the fetus, acting as an intermediary in the most important for the development of the baby processes: gas exchange, nutrition, removal of waste products. Through the uteroplacental blood flow, the baby receives blood enriched with oxygen, vitamins, minerals and water from the mother. Back through the placenta urea, creatinine, carbon dioxide are excreted.
The placenta is the “factory” of the hormones necessary to safely carry and give birth to a child. It produces hCG, progesterone, estrogen, placental lactogen. Without a sufficient level of these hormones, it will not be possible to carry the baby, and breastfeeding will be a big question.
The placenta begins to form after implantation of the ovum into the uterus. This usually occurs on days 8-9 after ovulation, if the egg is fertilized. At first, the placenta is preceded by chorion, thanks to which the blastocyst attaches to the functional layer of the endometrium of the uterus. Gradually, the chorion expands, new layers appear, and by the 14th-16th week of pregnancy the young placenta begins to perform its functions.
The “baby seat” grows and thickens until the middle of the second trimester, then the growth of the placenta stops, and its maturation or aging begins. Up to 30 weeks, the normal placenta has a zero degree of maturity, then it becomes more dense: deposits of calcium salts appear in it. Until the 34th week of pregnancy, the first degree, and after it (almost before birth) - the second. The third degree, which indicates that the placenta has almost completely exhausted its resources and capabilities, is recorded shortly before birth (during normal pregnancy).
Norms
Until the 20th week of pregnancy, the thickness of the placenta has no diagnostic value. “Baby seat” is determined by ultrasound, the place of its attachment is fixed, but the thickness will be measured only after 20 weeks. An ultrasonic sensor will determine the thickest part of the placenta, make a measurement - this indicator is considered decisive. It is important whether the thickness complies with the standard values for the current gestational age. The rates are shown in the table below.
Here is a table of placenta thickness by week.
Duration of gestation, (weeks) | The thickness of the placenta (range of normal values), mm |
20 | 16.7–28.6, usually - 21.9 |
21 | 17.4–29.7, on average - 22.8 |
22 | 18.1–30.7, on average - 23.6 |
23 | 18.8–31.8, on average - 24.5 |
24 | 19.6–32.9, usually 25.3 |
25 | 20.3–34.0, usually - 26.2 |
26 | 21.0–35.1, usually - 27.0 |
27 | 21.7–36.2, on average - 27.9 |
28 | 22.4–37.3, on average - 28.7 |
29 | 23.2–38.4, on average - 29.6 |
30 | 23.9–39.5, usually - 30.5 |
31 | 24.6–40.6, usually - 31.3 |
32 | 25.3–41.6, usually 32.1 |
33 | 26.1–42.7, on average - 33.0 |
34 | 26.8–43.9, on average - 33.8 |
35 | 27.5–45.0, on average - 34.7 |
36 | 28.0–46.1, on average - 35.5 |
37 | 27.8–45.8, usually 34.3 |
38 | 27.4–45.5, usually 34.0 |
39 | 27.1–45.2, usually 33.7 |
40 | 26.7–45.0, usually 33.4 |
Values are average. In practice, there may be minor deviations from these norms, and in each case the doctor makes an informed decision, starting from individual circumstances and peculiarities of pregnancy. However, obvious deviations, which are not limited to tenths of a millimeter, require additional examination. A thin placenta whose thickness is not more than 20 mm, or a thick placenta not exceeding 5 cm, is not normal.
If, in addition to the thickness of the placenta, which does not meet the deadline, there are no other pathologies and complications of pregnancy, it is usually decided to wait and watch. It is possible that the placenta has its own characteristics of the structure, and they should not inspire fear if this thickness does not affect the functionality of the "children's place".
Causes and consequences of deviations
Deviations from the norms are of two types: a thick placenta or very thin. Both are risk factors, because anomalies in the structure of the “children's place” violate its functions, on which the well-being and development of the baby directly depend. It is worth considering in detail both situations.
Thick
Placenta hyperplasia is referred to when the thickness of the “children's place” is above the upper limit of the acceptable range of normative values. The greater the difference, the more serious the situation. The thick placenta is alarming physicians much stronger than the thinned one, because with hyperplasia, the temporary organ ages faster, matures, and this is fraught with premature birth, fetal hypoxia, placental insufficiency and retarded crumbs.
If the placenta is aging ahead of time, the baby in any case loses oxygen, vitamins and nutrients. He may show symptoms of intoxication of the body, because the placenta copes worse and slower in excretion of waste products.
There are a lot of reasons that can cause hyperplasia of the “children's place”. This, for example, diabetes in the future mother. It affects not only the thickness, but also the structure of the placenta - an additional lobe may be present.
The thickness may be increased due to chronic anemia, which some pregnant women begin to experience in early pregnancy.
If a woman has a viral disease in the early period (for example, influenza or ARVI), the likelihood that placental hyperplasia will occur is very high. By thickening the “baby seat” can respond to infections of the genital tract, venereal diseases, as well as “winged” infections (chlamydia, ureaplasmosis and others).
At any stage of pregnancy, the thickness of the placenta may begin to increase due to Rh-conflict, if the Rh-negative mother bears a Rh-positive baby, resulting in sensitization. In the later stages, the hyperplasia of the “children’s place” threatens pregnant women with preeclampsia, edema, high blood pressure and overweight.
Functions of the placenta with thickening significantly deteriorate, especially the protective function. If hyperplasia is caused by an infection, such a placenta will not be able to protect the baby, it is more likely to become infected and may die in utero. The early stages of thickening do not make themselves felt. Only with the passage of ultrasound diagnosis is it possible to determine such a violation.
But at a later date, the development of the pathology of a woman will be “informed” of the baby's movement: he will begin to show great concern, and then episodes of physical activity will become more rare. On CTG can detect violations of the fetus, uteroplacental blood flow to the USDG will also be impaired.
Treatment is prescribed only after determining the exact cause of the anomaly. If it is an infection, a woman is prescribed a course of antimicrobial or antiviral therapy, diabetes is prescribed a standard course of treatment by an endocrinologist, with gestosis, hospitalization may be required, as well as a diet, normalization of blood pressure. Unfortunately, medications that could reduce the thickness of the placenta does not exist.
Women are recommended drugs to improve blood flow in the uteroplacental vessels. Most often used "Actovegin"And" Curantil. " In addition, vitamins and mineral supplements, iron preparations are prescribed.
In case of rhesus conflict, intrauterine transfusions may be performed.
Thin
If the thickness of the placenta for a given period does not exceed the values of the lower limit of the allowable range, they are said to be underdeveloped or hypoplasia of the “children's place”. The functionality of such a placenta is significantly limited, and only in one case it can be a variant of the norm: the woman herself has a fragile, slender body build and bears a small-sized baby. In this case, the development of the crumbs will not suffer.
In all other cases, an underdeveloped "children's place" can lead to negative consequences: hypoxia, delayed development, and the threat of death of the baby. A thin placenta is sometimes indicative of genetic abnormalities of the fetus. The risks of thinning the placenta increase after postponed early viral infections, as well as due to sexually transmitted diseases.
Preeclampsia in the second half of pregnancy is one of the most common causes of the development of hypoplasia, as is the presence of chronic kidney, heart, and thyroid diseases in a woman. To thinning often leads to smoking during pregnancy, as well as alcohol and drugs.
Usually with hypoplasia, there is a delay in intrauterine development of the baby. You can cope with the problem by using drugs that improve uteroplacental blood flow, vitamin intake, correction of maternal nutrition. If the causes are in developmental defects or chromosomal abnormalities of the fetus, it is not possible to eliminate IUGR.
Useful tips
Since there is no way to feel the thinning or thickening of the “children's place” on our own, a woman should regularly and timely visit her doctor during pregnancy, undergo all the necessary examinations, get tested and do an ultrasound scan. Refusal of the examination can be costly for the mother and her baby.
When detecting abnormalities in the thickness of the placenta do not need to fall into experiences - medicine has a sufficient arsenal of tools, techniques and medication to support the baby, to extend the gestation to the due date.
Avoid viral and infectious diseases during pregnancy, do not take medicines without a doctor's prescription, stop smoking and drinking alcohol, eat properly and be sure to monitor your blood pressure and weight.
The absence of risk factors reduces the likelihood of pathology of the placenta.
See what the placenta is for, what it is intended for, how it is located in the uterus, in the next video.