What is sperm morphology, what standards exist and how to improve performance?
At the planning stage of pregnancy, it is sometimes necessary to examine male germ cells. Unfortunately, in recent years, the number of men suffering from various forms of male infertility has been growing. Environmental factors, working conditions, bad habits, food affect.
About what awaits a man, if he was assigned not just a spermogram, but a spermogram with morphology, we will tell in this article. We will also touch on the issues of norms and deviations from them and find out how a man can improve his performance.
What it is?
Men do not like to admit that the cause of marital infertility may lie in them. However, the statistics is cruel - about 40% of infertile couples who have been trying to get pregnant unsuccessfully for 3 years or more deal with male infertility.
Therefore, when going to the doctor with complaints that the child “does not work”, a full and detailed examination is recommended not only for the woman, but also for her partner.
The main diagnostic method for the representatives of the stronger sex is a spermogram. In the course of this study estimated the number of male germ cells, their ability to move, structural features and other important parameters for successful fertilization.
The morphological study of sperm is one of the important components of a complete diagnosis. Without it, the picture of the processes in the spermogram will be inaccurate and incomplete.
The sperm morphology is carried out microscopically. With the help of modern high-precision equipment, the doctor divides all living and theoretically capable of conceiving sperm into normal and pathological. There are several methods for assessing the morphological features of the zinger. The most common is a study on the so-called "Kruger's strict criteria."
According to Kruger, spermatozoa undergo a rigorous selection for fitness. For conception, as you know, you need only one healthy and normal sperm, which can penetrate into the egg. But if there are more such healthy cells, then the chances of conceiving a child increase.
The Krueger evaluation system involves the selection of cells according to the following parameters:
- head width and shape;
- sperm neck width;
- shape and length of the tail;
- the ratio of the tail, the middle part and the head;
- the state of the cytoplasmic membrane of the germ cell;
- other features of the structure.
In conclusion, the Kruger Fertility Index is always indicated. It is expressed as a percentage, and decoding is not difficult even for people who are far from medicine.
If it is indicated that the Kruger Fertility Index is 22%, this means that 22% of morphologically ideal spermatodes were found in the sperm sample for analysis. They were the ones who were rigorously selected, compared with the existing standards and are ready for fertilization.
It is not always the only sperm with morphology is enough to establish the true causes of male infertility. Indicators of the study may be normal, and conception is still not possible to achieve.
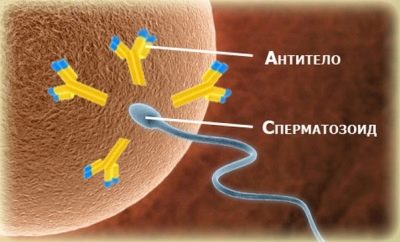
To make the picture more complete, a man may be advised to additionally make a so-called mar-test.
This is an immunological study that will show whether these morphologically ideal sperm cells are exposed to antibodies.
There are other tests:
- The EMIS test makes it possible to judge the functional abilities of male germ cells;
- biochemistry of sperm determines the errors in the metabolism of men and makes it possible to correct it;
- DNA fragmentation makes it possible to evaluate sperm from a genetic point of view.
How does the analysis, preparation
A man should carefully prepare for the survey. Doctors do not recommend having sex and masturbation for 3-6 days before delivery of the ejaculate. So the concentration of sperm will be the most informative for laboratory research.
A week before the analysis, a man should refrain from taking alcohol, antibiotics, hormonal drugs.
During this prep week do not bathe in the bath, relax in the sauna and sunbathe in the sun or in the solarium. Any thermal effect on the testicles can give unreliable results, since the number of normal and motile sperm decreases with heating.
A representative of the stronger sex can donate semen for analysis in two ways:
- To appear in a medical institution and by masturbation in a separate room to collect the material in a sterile glass.
- Collect material at home and deliver it to the laboratory. Home method can also be carried out by masturbation, this method is considered a priority.
You can ask the medical institution for a special condom without lubrication. In it, a man can have a full sexual intercourse. The seminal fluid collected in the condom should also be delivered to the laboratory.
It is desirable to transport the material in compliance with the temperature regime, which is closest to the temperature of the human body. For this you can purchase special medical thermocontainer. Some clinics provide such containers to their clients for free.
Sperm should be in the laboratory in the shortest possible time - within an hour.
Normal indicators of sperm morphology
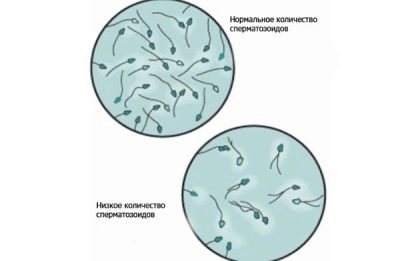
Generally, man is considered capable of conceiving in a natural way without the intervention of reproductive assistive methods, in the event that:
- about 20-40 million germ cells are found in his spermogram;
- total sperm volume of at least 2 milliliters;
- spermatozoa that are mobile and active, in this amount not less than 25%;
- if the number of spermatozoa that are not “rushing”, but moving directly to the target, along a straight path, is not less than 50%.
It is considered a good sign if the semen is detected not less than 15% of healthy, morphologically correct sperm.
The morphological assessment itself involves the analysis of the structure of germ cells. The strict Kruger criteria even regard the boundary parameters, which many other methods refer to as norm variants, as pathology. Even the slightest discrepancy between the sperm cell and the standard leads to immediate rejection of this cell.
The ideal sperm must meet several important criteria. Here they are:
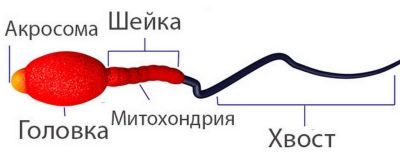
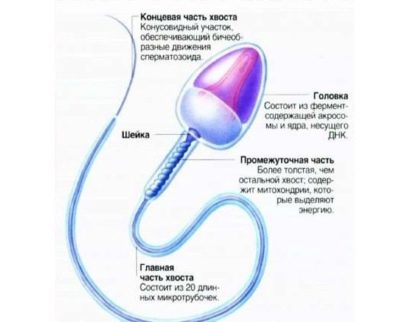
- Head. A sperm with a normal head morphology always has one head, not two and no more. Head shape is strictly oval. At least half of the head area should be occupied by an acrosome - a small space, an organoid. The normal width of the head is 2.5-3.5 microns, the normal length is considered to be a value in the range of 4-5.5 microns.
- Neck. This part of the male reproductive cell should not exceed 1 micron in width. The length of the neck should ideally be equal to a value not exceeding one and a half head length. The neck should be connected to the head at a ninety degree angle, correctly, without visible curvature. The neck itself should be flat.
- Tail. This part of the germ cell should occupy 90% of the total sperm size.The tail should be flat, not curved, not twisted, not having tubercles, nodules. It tapers slightly and sharpens at the end. In relation to the head, the tail should be 9-10 times larger. The tail of a healthy reference spermatozod in the presence of only one, not two and not three.
Abnormalities and causes
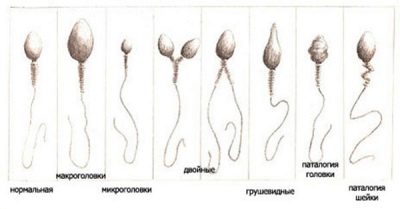
Sperm with pathological morphology look like this:
- Head defects. Anomalies can be manifested by a change in shape from oval to round, resembling eight, oblate, pear-shaped. The acrosomal area can be reduced, filled with vacuoles. Head sizes too large in comparison with the norm and significantly reduced are also considered signs of unsuitability and inconsistencies. Two or more heads in a single cell is a mutation that excludes sperm from the number of healthy cells.
- Cervical defects. Spermatozoa with an abnormal neck initially look different from the norm. It is the defects of this part of the cell that strongly distort its appearance. The neck can be twisted, thickened, inhomogeneous, thinned beyond measure. It can be attached to the head is not at a right angle, and sweat blunt or sharp, which creates a visual effect of "twisted" sperm.
- Anomalies of the tail. Usually, among the cells with poor morphology, spermatozoa lacking a tail, with a short or too long tail, with a tail that is partially broken, are found. If the tail part of the genital cell is not at right angles to the head, if the tail is twisted, bent in any direction, the sperm cell cannot be considered normal.
- Other defects. In a sperm sample, lab technicians can only find tails. This becomes possible when the head and neck are loose. In this case, the sex cells are attacked by Sertoli phagocytes, and the heads do not withstand this. Only tails remain. Analysis with poor morphology, when the number of healthy sperm is less than 14-15%, is the basis for the establishment of teratozoospermia.
The chances of natural conception in such men are reduced by exactly as much as the number of abnormal cells is increased. In addition, there is a chance to conceive a child with gross chromosomal abnormalities.
A critical level of reduction in healthy cells that meet the Kruger criteria is considered to be 4%. In this situation, it will be difficult to fertilize an egg, even in test tube conditions for IVF. But modern medicine is not worth it, and even men, whose Kruger fertility level is at 2-3%, are not deprived of the opportunity to become dads.
For this they may be offered ICSI methodin which even in the pathological sperm of a sterile man, the doctor will be able to find a single healthy and standard-compliant sperm cell, introduce it directly to the egg and then plant the fertilized egg.
Among the most common causes of teratozoospermia are:
- Acceptance of hormones. Most often this cause is found in athletes who take steroid hormones to regulate body weight. Sometimes sperm becomes unsuitable for conception from a morphological point of view due to the fact that the man received long-term hormonal treatment.
- Violation of hormonal background. Due to various diseases, including metabolic pathologies, the ratio of hormones, including sex hormones, can vary in the body of a man.
- Viral infections. The sperm morphology can be influenced by both the influenza virus and SARS (due to high temperature), but the most serious malformations of germ cells are caused by the second type of herpes virus, the so-called genital herpes.
- Inflammation of the genitals. Any inflammatory disease of the male reproductive organs, including such widespread prostatitis, can cause changes in the morphology of sperm.
- Lifestyle.If a man abuses alcohol, drugs, smokes a lot, does not eat properly or is undernourished, the risk of teratozoospermia increases.
- Working conditions and other factors. If the activity of the representative of the stronger sex is associated with exposure to radioactive radiation, high temperatures, then mutations of spermatozoa can be explained precisely by these factors. The region of residence also plays a role - in areas with an unfavorable ecological situation, the facts of male infertility are much more common.
- Prolonged stress This is also one of the most common causes of the pathological morphology of sperm. In the 21st century, it sometimes comes out on top.
Ways to improve sperm quality
In order to increase the fertility of a man, it is necessary to find the true reason why spermatozoa in him began to acquire pathological morphology. If this is inflammation, then treatment begins with anti-inflammatory drugs. If the cause is in the herpes virus, the treatment will be based on antiherpetic drugs.
Psychotherapists will help men who have developed teratozoospermia against the background of long-term strong nervous stress, to restore their reproductive abilities.
For those whose blood tests show hormonal disruptions, an endocrinologist will prescribe treatment, which will be based on the type of imbalance and the actual amount of certain hormones.
Regardless of the reason, all men are recommended to take vitamin complexes, folic acid, preparations of zinc and selenium, vitamins A, E, B, D, C.
Curing teratozoospermia will help and avoiding bad habits, limiting alcohol and nicotine.
Men with impaired sperm morphology are recommended to change the situation - for several months to live outside the city, away from gas pollution and other adverse factors. Sometimes only this measure can significantly improve the results of the analysis and increase the chances of the family to conceive the long-awaited baby.
To improve the quality of germ cells, one should responsibly approach the organization of food, exercise, adjust the work and rest regime, avoiding “distortions” in it, if possible, give up work at night, as well as labor “feats” overtime.
A man should definitely get enough sleep, taking to sleep at least 8-9 hours a day. It makes sense to do sports such as swimming, running, skiing. Any physical activity in the fresh air will only benefit.
How to improve sperm performance, see the next video.