The norms of spermogram, interpretation of indicators and causes of deviations
Men's health to conceive a child plays an important role, not inferior to women's health. Unfortunately, this fact is often underestimated by the representatives of the stronger sex, so the statistics sound scary - about 40-45% of all infertile couples cannot conceive a baby precisely because of male infertility. That is why pregnancy planning is most reasonable to begin with a semen.
In this article we will explain what this analysis is and how to decipher it.
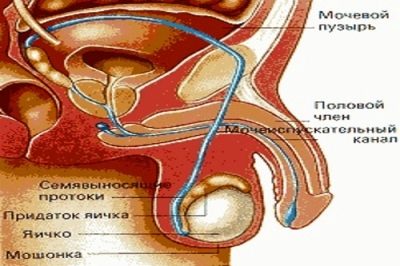
The essence of the study
Spermogram is a quantitative and qualitative analysis of the ejaculate, which is carried out mainly microscopically. Under laboratory conditions, the study determines the main characteristics of the male seminal fluid. They may indicate reproductive health problems, inflammatory processes of the future genitourinary system of the pope.
According to the results of spermograms, one can make a fairly accurate conclusion about the ability of this man to fertilize.
Bad spermogram - not a sentence yetBecause modern reproductive medicine does not stand still and can offer many auxiliary methods to couples who cannot conceive a child due to the inappropriate quality of sperm, pathological forms of male germ cells.
Types of analysis
When conducting spermograms, the doctor takes into account the essence of the patient's treatment. Sometimes it is quite enough to make a basic spermogram, which will include an assessment of the quantity and quality of germ cells.
However, there are situations when the basic research shows good results, and conception does not occur in a woman without problems. In this case, the doctor prescribes an extended spermogram, within which the sperm morphology is evaluated - their appearance, compliance with reference standards.
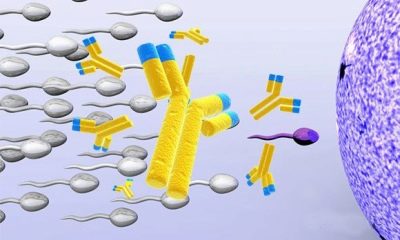
Sometimes there is a need for spermogram with DNA fragmentation, research with biochemistry, MAP test. The indication for the latter is immunological infertility - a condition in which antibodies to sperm are produced in the body. It is they who destroy live and motile sex cells, not allowing them to fertilize an egg. Extended spermogram is always more informative.
The analysis is usually prepared from 1 to 3 days depending on the workload of the laboratory of the selected clinic. The conclusion is given to the patient on his hands, it is a completed form with an indication of all defined indicators and individual values.
Deciphering should deal with a doctor, but for special curious men and their wives, we are ready to tell you how to decipher the spermogram yourself.
And now we look at what sperm looks like under a microscope with comments from a urologist.
Full transcript of the results
The conclusion form usually contains the following parameters.
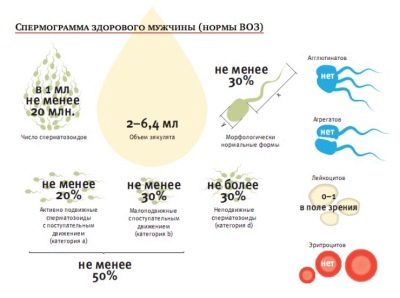
Volume
This refers to the amount of sperm that is provided for analysis. According to WHO standards, which are currently the only standard in the world for spermograms, an amount of less than 1.5-2 ml is considered pathological and makes research very difficult.
The fact is that the amount of ejaculate is influenced by the amount of prostate gland and seminal vesicle fluid. If there is not enough of it, then this is a reason for additional research of the state of these organs. Small sperm reduces chances of conceptionSometimes it is impossible to conduct a study precisely because of too little material.
An insufficient amount of sperm can be associated with frequent sex life, so it is recommended to abstain from sexual contact for several days before semen.
Colour
Usually sperm has a white, milky, grayish, pearl, opal shade. In conclusion, most often they write that the color of the material is “whitish-grayish”. What the ejaculate color can tell, the doctors themselves, for the most part, do not know, because this indicator, although it is listed as part of the main indicators, has no diagnostic value.
The analysis of sperm under a microscope allows you to accurately judge the cellular composition, so the color change to pinkish, if there is blood impurities, or greenish, if there are impurities of pus, it is not necessary to mark separately. Just the color is always included in the assessment of the ejaculate, and this graph exists in a modern form rather as a tribute to traditions.
Smell
Almost the same story happened with the smell. This item is in the conclusion, but its diagnostic value is not entirely clear. Some doctors claim that indirect effects on the health of the prostate gland can be made by smelling the ejaculate. However, there is no conclusive evidence.
The smell, like color, is indicated in the spermogram results because it has always been like this. Usually the smell is described as specific pronounced or specific mild.
Consistency
This part of the report describes the physical property of sperm as viscosity. After ejaculation, seminal fluid is thick enough, it gradually dilutes.
Increased viscosity can create problems for the movement of germ cells.
In order to determine the viscosity, the laboratory assistant lowers a glass rod into the sperm sample, lifts it above the laboratory container and looks at the length of the resulting “thread”. The more viscous the sperm, the longer this "thread".
Normally, this parameter should be less than 2 centimeters, that is, the length of the residual "thread" must not exceed this value. If the "thread" has a length of 2 centimeters or more, the sperm is considered thick and viscous. In conclusion, if a man is normal with this parameter, it is indicated - “weakly viscous” or “moderately viscous”.
Liquefaction time
This column indicates the time during which sperm is diluted. Usually this time interval varies between 15 minutes and 1 hour. If after 60 minutes the sperm does not liquefy, it usually remains so. The laboratory assistant has to add special enzymes to it in order to conduct all the other tests and tests.
The interpretation of this parameter is quite simple. If the column indicates 20 or 30 - this is the time in minutes, which passed to liquefy the material. 15 to 60 minutes is the norm.
Acidity
Like any other liquid medium of the human body, sperm has its own acidity. Usually in healthy adult men, the acidity level of the ejaculate is in the range of 7.5-8.2.
The normal is pH above 7.2. If the sperm has less acidity, the ability to conceive in this man is reduced, because it becomes more difficult for sperm to dissolve the egg cell membrane in order to penetrate it.
Sperm concentration
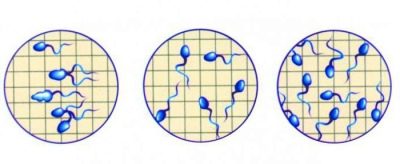
The concentration of spermatozoa is determined in 1 ml of liquid. To calculate them, you need special equipment - sperm analyzer or counting chamber. Less commonly, laboratory technicians use the smear method when 1 drop of sperm is applied to a laboratory glass with a size of 22x22. Then the microscope is tuned to the increase in X400 and consider how many sperm will be in sight. The same amount, only in millions, will be inherent in 1 ml of liquid.
Example: 25 spermatozoa were in sight, which means that there are 25 million of them in 1 milliliter. Normal concentration, favorable for fertilization - from 20 million per milliliter.
Total sperm count
This column indicates how many germ cells are present in the total volume of seminal fluid provided for the study. As well as concentration, this part of the sperm is considered one of the most informative in terms of identifying the causes of male infertility. The total counts counting chamber or sperm analyzer.
Knowing that a normal concentration of 20 million per milliliter is considered, the reference value is displayed. If a man has passed 3 milliliters of sperm (see the “Volume” item), then 60 or more millions of “zinger” will be the norm, if the volume is 2 milliliters, then the rate starts from 40 million cells.
This part of the report also indicates the figure. The higher the number of germ cells in seminal fluid, the higher the chances of conception.
Mobility
In the ejaculate, sperm cells of four types of activity are counted. The most mobile, aspiring only directly, receive category A from the laboratory technician and are considered the main applicants for fertilization.
No less progressive, moving in the forward direction, but their slightly slower counterparts receive category B.
Male sperm is considered suitable for natural fertilization, if it contains at least 25% of “zhivchikov” type A or the number of cells of types A and B in the sum is equal to half of all spermatozoa. With this result, no problems with fertility in men are observed.
Sperm cells that move sluggishly, spin in one place, rush about randomly in different directions, get category C, and fixed cells - category D.
In conclusion, category names are not always indicated. Sometimes the doctor refers to the percentage of active motile sperm (this is types A and B), sedentary (type C cells) and fixed (type D cells). In this case, the rules are similar.
Actively mobile should be at least 50%. If so, you can ignore the rest.
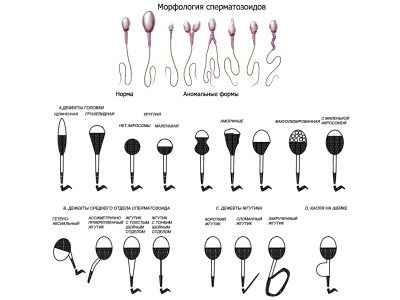
Morphology by Kruger
Extended spermogram implies a mandatory assessment of the morphological features of the male germ cells It is understood that in a healthy sperm must be a sufficient number of cells of the correct form with a normal structure. For this sperm is compared with the standard.
Kruger's assessment criteria are the toughest, any deviation from the norm, even if it is single, according to these criteria, is considered a pathology, and spermatozoa are rejected:
- The sperm head should be flat, oval. Any other forms are considered abnormal.
- The sperm neck should be positioned correctly, and the tail should not bend and wring, twist.
- Each part of the sperm is to be measured, the proportions of the cell body are compared.
What a healthy cell looks like, is described in detail in the Kruger method, it is with these parameters that the sample under test is assigned.
Violations:
- one or more heads;
- one or more tails;
- no head or tail;
- curled tails;
- an uneven middle part and a thin flimsy neck, which can not hold the tail;
- pathology of the head structure;
- wrong flagella attachment angle.
Morphology is easy to decipher.The laboratory calculates reference, ideal for fertilization, sperm and bad, inappropriate to the selection criteria. The resulting value of "good" cells is called Kruger index.
If the conclusion indicates that the Kruger fertility index is 14-15% or more, this means that the content of reference sperm in seminal fluid is at the level of 14-15%, which is the lower threshold of the norm.
Cell viability
The number of sperm in the ejaculate may be normal, but conception does not happen anyway. The reason may lie in the viability of the cells. If the genital cell moves, it is always alive, but if it is motionless, then it can be both alive and dead. The more live cells in the ejaculate, the greater the chances of a man becoming a dad. It is considered normal if the semen contains more than half of live gametes.
To find out which sperm are alive and which are not, the lab technician can tint a drop of sperm with a laboratory dye eosin. A living cell will remain of normal color, since its membrane is intact and reliably protects it from the dye entering the cell. Dead sperm will be pink, because their death is always accompanied by deformation and perforation of the membrane.
Also, the number of dead sperm is calculated after placing the sample of seminal fluid in a hypotonic solution. Healthy living sperm swell from him, their tails are bent in an arc, the dead do not react to the nutrient solution. The conclusion indicates the number in percent. This number indicates the content of living cells in the ejaculate.
Spermatogenesis cells
These cells belong to the category of round cells (round cells), since they are not spermatozoa and are devoid of tails. These are just future spermatozoa, which have to go through several stages of development, before they turn into full-fledged germ cells. They are also detected in semen by microscopic examination.
Normally, in a healthy adult male, the ejaculate contains about 2-4% of such still-mature young germ cells.
Excess rates can talk about a variety of pathologies, mainly related to the process of development and maturation of sperm.
White blood cells
A small number of leukocytes in the field of view of a technician is normal. There is nothing wrong with that 1 ml of semen contains up to a million white blood cells. This is the norm.
However, if the number of cells exceeds this norm, this indicates an inflammatory process in the reproductive system of the man. Therefore, the entry in the conclusion of "leukocytes - 1-2 in p / zr" should not cause concern - there are no inflammatory and infectious processes with this result.
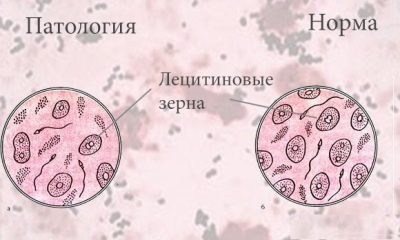
Lecithin grains
They must be present in healthy semen. Lecithin granules or lipoid bodies (they are non-cellular formations) are part of the secretion of the prostate gland, therefore, their decrease indicates problems with the prostate.
Normally, lecithin grains are contained in an amount of about 10 million in 1 milliliter. In conclusion, their number is not indicated in numerical or percentage terms, usually the description looks quite generalized - “norm” or “moderately”.
Slime and Macrophages
The appearance of mucus, clots in the semen is always a very disturbing symptom, which can indicate a strong inflammatory or infectious process in the organs of the reproductive system.
Large cells - macrophages in norm can be in single quantities in the field of view. An increase in their number is also a sign of infection.
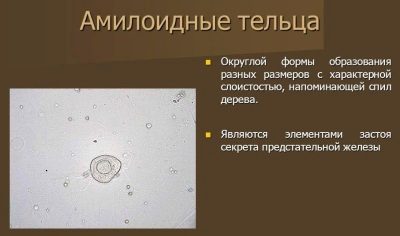
Amyloid bodies
Amyloid bodies, resembling starch in their structure, appear in semen when pathological processes occur in the prostate gland.
The appearance of amyloid formations in the ejaculate suggests that a man develops prostatitis, prostate adenoma and other ailments.
Simultaneous detection of macrophages and amyloid bodies can indicate the development of prostate adenoma.
Sperm Agglutination
The term "agglutination" refers to the process of bonding. In this case it is meant gluing sperm cells together. Such cells cannot participate in fertilization.
The causes of this pathology can be varied, most often this phenomenon is observed in immunological infertility. In the normal process of agglutination during the semen should not be detectedwhat the conclusion says is “not detected” or “not detected”.
Antisperm antibodies (MAP test)
Antibodies to spermatozoa can be produced in the female and male bodies. If their number is large, then they begin to destroy the male sex cells that are completely healthy and ready for fertilization. Sperm heads or tails are affected. Damaged cells stick together, aggregation occurs, and gamete motility is impaired.
The MAP test is based on the addition of rabbit antibodies to human antibodies in sperm. If the injected drug begins to adhere and envelop spermatozoa, we are talking about the presence of antibodies and immunological infertility.
Standards in the table (normospermia):
The main indicator of semen | Amended WHO rules of 2010 | WHO standards until 2010 (for reference) |
Volume | Not less than 1.5 ml | Not less than 2 ml |
Acidity | Not less than 7.2 | Not less than 7.2 |
Sperm concentration | Over 39 million in total, at least 15 million in 1 ml of material | Not less than 20 million in 1 ml., Not less than 40 million in total |
Mobility | Not less than 40% of cells A and B, more than 32% of cells of type A | 50% of type A and B cells, or 25% of type A cells an hour after ejaculation |
Viability | At least 58% of living cells in the sample | At least 50% of live sperm |
White blood cells | Not more than 1 million per 1 milliliter | Not more than 1 million per 1 milliliter |
Antisperm antibodies | Not more than 50% of the test results | Associated with antibodies in the MAP test is not more than 50% |
Sperm morphology | At least 4% of healthy cells | 15% of morphologically healthy cells, at least 4% |
Pathologies
What kind of pathological conditions spermogram can tell, it becomes clear from the very name of these pathologies:
- Oligospermia - sperm concentration in seminal fluid is below normal.
- Asthenospermia - impaired motility of germ cells. Spermatozoa, which could quickly make their way in a straight line to an egg that is awaiting fertilization, have little or no.
- Teratozoospermia - the sperm morphology is impaired. There is a large number of ugly, mutated germ cells that are not capable of fertilization, and if they succeed, then the risks of genetic abnormalities in the fetus are high. Such a pathology is said when the Kruger Fertility Index is less than 4%.
- Azoospermia - the absence of sperm in seminal fluid. In this condition, the fertility of the man is absent, it is a severe form of infertility.
- Aspermia - the absence of sperm at all. In this case, the man may be reduced or may have no body sensations at all.
- Leukocytospermia - the presence of a large number of leukocytes in the seminal fluid. Regarded as a sign of infection or inflammation, is not directly related to fertility.
- Necrospermia - the absence in the sperm of live spermatozoa completely or the presence of too few live cells.
- Akinospermia - the absence of motile sperm in the semen. They can be alive, but with motor function they have significant difficulties. It differs from asthenospermia in its severity and severity.
- Cryptospermia - a negligible amount of sperm in the ejaculate. Microscopic and hardware calculation of their number is not subject.The material is subjected to centrifugation, and if then a small amount of sperm is detected in the sediment or it is not detected, then it is a question of cryptospermia.
- Hemospermia - the presence of blood in the sperm. Red blood cells should not normally be present in seminal fluid. Blood impurities are a very alarming symptom of serious diseases of the reproductive system.
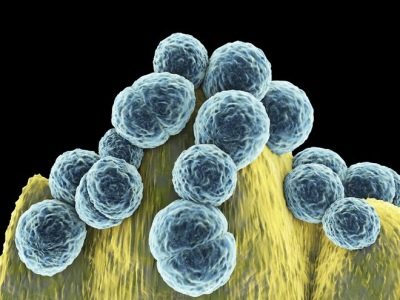
- Bacteriospermia - detection of a large number of bacteria in the semen. These can be cocci, for example, staphylococcus, Staphylococcus aureus, streptococcus, entercoccus faecalis, and other opportunistic pathogens. Such a picture may indicate the presence of a bacterial infection.
Causes of deviations
The reasons for which the results of sperm may disappoint a man and his soul mate, many. Most often, the factors affecting the semen indices are rooted in an inflammatory or infectious disease. These include untreated inflammatory diseases of the urogenital system, sexually transmitted diseases, sexually transmitted infections, ureaplasma, mycoplasma, chlamydia, etc. that are not cured in time.
Sometimes these diseases, called “winged” by the people, occur without any symptoms at all, so a man may not even be aware of the presence of, for example, chlamydia.
A roughly equal number of poor spermogram results also occur in men who have inflammatory diseases of the seminal vesicles and prostate gland, in which epithelial cells that produce sperm cells are affected.
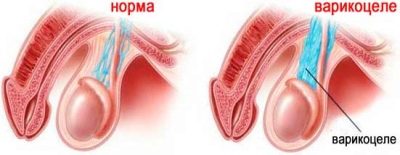
Often the cause of the violation of the quality of sperm is varicocele. Herpes sores are very dangerous in terms of the likelihood of infertility.which causes mutations and changes in the morphological structure of germ cells, as well as mumps (parotitis), transferred by the boy in childhood.
Even a simple flu virus or ARVI affects the sperm condition, but their influence is temporary, and the semen composition returns to normal within 2-3 months. However, this should not be forgotten, intending to pass spermogram.
Among the "painful" causes, the last place is occupied by the consequences of injuries and surgical operations. If a man suffered an injury to the brain or spinal cord, if operations were performed on these organs, if there were surgical interventions on the liver and kidneys, then the likelihood that the quality and quantity of sperm will become worse is great. Fights, blows "below the belt" - all this does not pass without a trace for men's health.
More rarely, the causes of violations identified during the examination lie in congenital pathologies - absence of testicles from birth, absence of vas deferens, defects and abnormalities of the structure of reproductive organs. Such reasons are usually unavoidable.
Even modern methods of reproductive auxiliary medicine can offer nothing to a man whose infertility is natural, a natural fact from birth.
The quality of sperm is much worse in men who live in large polluted cities with a deplorable state of ecology.
The male fertility is strongly influenced by his lifestyle. If the representative of the stronger sex works a lot, especially at night, and rests a little, if he abuses alcohol, drugs, smokes a lot, all this leads to a violation of the sperm morphology and other deviations in the spermogram, indicating that the male reproductive function is reduced.
At risk of male infertility are lovers of frequent trips to the bath and sauna, lovers warm up in the sun and visit the solarium, as well as men who daily for a long time use heated seats in the car. Thermal effects on the scrotum and the sex glands located in it have a negative effect on all processes of spermatogenesis.
The cause of problems with sperm quality may lie in long-term stress factors that a man is experiencing, as well as hormonal problems in his body, for example, problems with fertilization begin when the balance of thyroid gland hormones, as well as sex hormones, is disturbed, for example, testosterone .
Hormonal imbalance can begin with the treatment of hormonal drugs, as well as the use of steroid drugs to achieve athletic performance.
Anomalies of sperm and dysfunction of spermatozoa can also be caused by genetics, if the boy received from his parents a “defective” gene responsible for reproduction.
Treatment and prognosis for conception
If pathological forms of semen are detected, the man will need additional diagnostics. He will have to consult an andrologist and also visit other specialists - an endocrinologist, a surgeon, a neurologist and, possibly, a psychotherapist, if no objective medical reasons are established.
He is prescribed additional tests - blood, urine, ultrasound of the prostate gland, manual examination of the prostate.
Treatment begins after the cause is found. If reproductive abilities have decreased due to inflammation, infection, prostatitis, anti-inflammatory treatment with antibiotics will be prescribed.
If the cause is a varicocele, surgery may be indicated.
Hormonal problems are detected by analysis of blood for the concentration of different hormones, the therapy is prescribed by the endocrinologist.
All, without exception, the representatives of the stronger sex with problem semen It is recommended to revise your work schedule, stop working at night, start to get enough sleep. Sometimes it is beneficial to change the situation - moving from the city to the city, where the air is cleaner and the environment is better.
Alcohol, drugs and smoking are contraindicated. But without exception, regardless of the cause of infertility, vitamin preparations are prescribed, which include vitamins A, E, C, D, vitamins of group B, folic acid, as well as zinc and selenium.
There are ready-made complexes, created specifically for men planning to conceive. Vitamin therapy should last at least 3 months, so much time lasts spermatogenesis.
In the diet of men necessarily include foods rich in proteins - meat and fish dishes, dairy products, fresh greens (as a source of folic acid), nuts.
A man is not recommended to wear tight fitting underwear, and in the summer - synthetic pants and shorts, in which the scrotum overheats. In winter, hypothermia of the genitals should be avoided.
A man who plans to conceive a child is recommended to change his usual rest at the TV on weekends to active leisure - skiing, easy jogging, swimming. Visiting baths and saunas is reduced to a minimum or they are temporarily abandoned altogether.
Sexual life should be conducted taking into account the personal recommendations of the urologist-andrologist, who will tell you the best mode based on the sperm: if the sperm is too thick - more frequent sex, if it is liquid, then sex should be somewhat less.
Forecasts for conception are favorable even with serious violations of the spermogram. Medicine today can offer many ways to solve the problem - this is IVF and ICSI. In 97% of cases of acquired infertility can cope with it. Adverse prognosis only in the case of congenital and genetic abnormalities.
How to prepare a man for conceiving a child, see below.