What pathological forms of sperm are and how they affect the success of conception?
Men's health when planning pregnancy plays a very important role. If spermatozoa have pathological forms, then this can significantly affect the possibility of the natural conception of a baby.
Norm
In order to understand how the pathological forms of sperm form and look, you should first talk a little about normality. A sperm cell is a sex cell that has a single chromosome set and is necessary for fertilization, and therefore for procreation.
Sperm have a very small size - about 55 microns. Each male sex cell consists of three sections: the head, body and tail. The sperm head is shaped like an ellipse. It is slightly wider than other sperm sections. All this makes it resemble a tadpole.
The basic genetic information that will be transferred from the father cell to the daughter cell is located in the nucleus. Each sperm cell has a sex chromosome. It can be either X or Y. It depends on what sex chromosome the child gets, and its sex will depend. For the birth of a boy, a Y-chromosome is needed, and for the birth of a girl an X is needed.
Another very important element of the sperm is the acrosome. This cellular organ is a modified Golgi apparatus. In the acrosome there are special substances that are necessary for fertilization. With their help, the outer wall of the mature egg is affected. The acrosome has a size of approximately half the nucleus.
Scientists have found that there are about 15 lytic enzymes in the acrosome, which dissolve the outer shell of the egg. The most important of them is acrosine.
The head of the sperm ends with a neck - a special constriction that separates it from the middle part of the body of the sperm. Behind it is a moving tail. In the middle of the sperm are special formations, microtubules and mitochondria. They are necessary for the formation of a special substance ATP, necessary for the implementation of active movements of the sperm.
With the help of the rolling tail, the sperm can move. The most characteristic direction of its movement is around its own axis. Scientists have established and the average speed of movement of male germ cells: it is usually 0.1 mm per second.
It is believed that at this speed, sperm can reach the fallopian tube of a woman a couple of hours after the end of sexual intercourse.
In order for fertilization to occur, the sperm must travel a rather long way. On average, it is about 20 cm. The trajectory of sperm in the female genital tract is quite simple: they move from the outside inwards towards the fallopian tube.
Such biological features of the structure and functioning of sperm cells are necessary for the conception of a child to occur naturally. Impaired functioning or anatomical defects may contribute to impaired reproductive function in men.This may affect the formation of male infertility.
Types of anomalies
The development of scientific technologies made it possible to determine the most diverse pathologies in men. Every year, hundreds of studies are conducted aimed at studying spermatogenesis. This contributes to the fact that each year new pathologies are determined that can impair male fertility.
Various clinical signs are used to assess the pathology. So, for this are determined:
- the total length of the spermatozoon, as well as the dimensions of its main parts;
- total ejaculated sperm;
- total sperm count per ejaculate;
- sperm motility and viability;
- anatomical form.
After a comprehensive analysis, doctors can determine the presence or absence of pathology. If no pathological changes were detected, the diagnosis of “normospermia” is established. In this case, the reproductive function of the man is preserved, and he can become a father.
Doctors distinguish several clinical variants of the pathologies of spermatozoa. Usually, all pathologies are divided into several similar groups according to the main studied characteristics.
Reduction in the total number of male germ cells
One of the typical examples of this type of pathology is oligozoospermia. In this pathology, the sperm content in the ejaculate is below normal values.
If during the examination of spermatozoa in the ejaculated sperm were not detected, then this pathological condition is interpreted by doctors as azoospermia. This, as a rule, is a rather complicated pathology, which requires mandatory participation in the treatment of the andrologist.
Aspermia is a pathological condition in which not only spermatozoa, but also immature spermatogenesis cells are not detected in the studied ejaculate.
If, however, during the examination spermatozoa were still found, but are dead, then this condition is called necrospermia. It is extremely unfavorable for the implementation of natural conception. In this situation, male reproductive function is significantly reduced.
Sometimes when carrying out the centrifugation of the test ejaculate, specialists can detect a small amount of sperm. This pathological condition is called cryptospermia.
Mobility impairment
If the sperm are “lazy” and do not move well, then this condition is called asthenozoospermia. It is characterized by a decrease in physiological mobility below the norm.
In some cases, a man can develop several pathological changes at once. An example of such a pathology is oligoastenoteratozoospermia. This pathology is characterized by:
- a general decrease in sperm concentration in the ejaculate under study;
- approximately halving the number of sperm that can fertilize an egg;
- a decrease of almost two times the number of spermatozoa with straight-line movement.
Oligoasthenotheratozoospermia is one of the pathologies leading to the development of male infertility. Usually it comes to light spontaneously - when visiting couples who have been unsuccessfully trying to conceive babies for a long time.
In order to assess the functional disorders that have occurred, in addition to spermograms, doctors may also prescribe a testicular ultrasound test, laboratory tests for the detection of hidden infections and other studies. After a comprehensive diagnosis, an individual treatment plan is drawn up, aimed at improving well-being and restoring lost reproductive function.
Another pathology associated with impaired motility of spermatozoa is acinomasmia. According to statistics, it occurs in 30% of men. Akinospermia can be both total and partial.
The more inactive sperm in the semen, the higher the risk of developing male infertility.
Anatomical defects of the structure
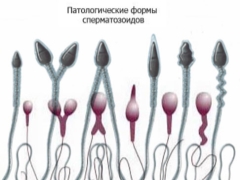
Various abnormalities may be associated with impaired sperm.So, the shape of the head of the sperm may be incorrect or deformed. In a number of pathological cases, the sperm head may be conical or pear-shaped. There are even abnormal two-headed sperm.
Head sizes may be excessively large or small. Such pathologies, as a rule, are accompanied by a violation in the structure of the acrosome: it can be too small, vacuolation or asymmetrical.
Specialists identify a number of pathologies associated with changes in the anatomy of the cervix sperm. So, she may be bowed. In this case, the angle that forms between the head and the neck of the sperm is more than 90 degrees. Also, the neck may be asymmetric or excessively thin.
Defects tails sperm can be very different. So, the tails can be numerous, too short or, conversely, fairly thickened, and also have a completely twisted end. Such anomalies contribute to the fact that although the sperm cell remains viable, it cannot fully perform its biological function.
Normally, sperm have a negative charge. This is necessary so that they repel each other, and their gluing does not occur.
If, for some reason, this balance is disturbed, sperm adhere or stick together. In such a situation, the possibility of natural conception decreases many times.
Causes of anomalies
Doctors distinguish quite a lot of various causal factors that can provoke the development of various pathologies in men. They can be either congenital or acquired. The severity of adverse symptoms depends largely on the severity of the pathology.
A common cause of the emergence of various pathologies of spermatogenesis in men are the consequences of infectious diseases. A long-term infection that develops in the urological tract also contributes to inflammation in the reproductive organs. Especially often recorded diseases that are sexually transmitted.
Defective spermatozoa can also be caused by various traumatic injuries of the intimate organs. Spinal cord injuries can also cause the development of a number of pathologies. Violation of the nerve impulses from the genital organs to the cerebral cortex due to such diseases leads to the development of erectile dysfunction, and therefore, can cause the development of male infertility.
The quality of sperm also largely depends on the age of the man. It is believed that younger men have much less pathological forms of sperm. And also in men up to 40-50 years, spermatogenesis proceeds quite intensively. With age and the accession of concomitant diseases, indicators of male health decline.
Andrologists note that uncontrolled long-term medication has led to the development of a number of urological disorders. It is believed that some alpha-blockers may lead to the development of aspermia. Typically, these tools are used to treat benign prostatic hyperplasia.
Pathologies associated with impaired motility of sperm can be caused by various psycho-emotional stresses. The stronger the effect, the brighter the adverse symptoms may appear. Constant exhausting stress at work helps to reduce reproductive function in men.
The development of pathologies of spermatogenesis can lead a variety of reasons. Without their definition, doctors cannot conduct a comprehensive treatment of the resulting disorders.
Diagnostics
The main diagnostic method to determine the various defects of spermatogenesis, is the spermogram. Currently, this study can be done in many medical institutions.Before passing the examination, doctors recommend men to limit sex life 3-7 days before the date of analysis.
In addition, before taking the survey should not drink alcoholic beverages and use the sauna. Intensive loads in the gym should also be limited a few days before the laboratory test.
Immediately after the delivery, the ejaculate is a rather viscous mass. Then he gradually liquefies. As a rule, it takes from 15 to 60 minutes. This time period is also estimated by experts and is called the “liquefaction time”. If after an hour the ejaculate does not become sufficiently liquid, then it is diluted with the help of special proteolytic enzymes.
After preliminary preparation, the basic morphological properties of the ejaculate under study are determined. With the help of modern microscopy, the specialist conducting the study evaluates the size, shape, mobility, viability and other properties of sperm.
After the study, a medical report must be compiled, in which all the data are entered. Further, with such a conclusion a man should seek the advice of a doctor-andrologist.
How is it treated?
A treatment plan for spermatogenesis abnormalities is always made individually. To do this, the initial cause that led to the development of the pathology, as well as associated diseases that are present in each case, are taken into account.
With many pathologies, several treatments are required.. Full complex therapy is necessary to improve the general condition of the man, as well as to normalize his reproductive function.
To improve spermatogenesis, drugs can be selected that have an effect on the work of the prostate gland and testicles. Some of them are hormonal. When using these drugs is very important to remember that they have a number of contraindications. These funds should be written out only by a doctor, since self-prescription and uncontrolled use can only aggravate the situation and not lead to improvement.
Multivitamin complexes are also capable of improving male health outcomes. They can be assigned as a long-term, and on course admission. Psycho-emotional stress, malnutrition and destructive habits lead to a decrease in the required concentration of beneficial vitamins and microelements in the blood.
Vitamin-mineral complexes help to fill this deficiency and significantly improve spermatogenesis.
For information on the pathological forms of sperm and how they affect conception, see the following video.